2. Healthcare Benefits
The objectives of this chapter encompass a comprehensive exploration of healthcare benefit programs, spanning historical context, structural intricacies, design considerations, cost containment strategies, and emerging trends. The specific aims include:
Presenting a Brief History of Healthcare Benefits:
Unveiling the historical evolution of healthcare benefits to provide a contextual foundation.
Explaining the Structure of Healthcare Benefit Plans:
Delving into the intricate architecture of healthcare benefit plans, elucidating their components and organizational frameworks.
Discussing Design Issues Related to Healthcare Benefit Plans:
Analyzing the nuanced considerations involved in crafting effective and employee-centric healthcare benefit plan designs.
Evaluating Cost Containment Issues Related to Healthcare Benefit Plans:
Scrutinizing strategies and mechanisms aimed at curbing costs within healthcare benefit plans without compromising quality.
Introducing Consumer-Driven Healthcare Plans:
Unveiling innovative approaches such as consumer-driven healthcare plans, exploring their principles and implications.
Discussing the Accounting Implications of Healthcare Benefit Plans:
Examining the financial accounting intricacies associated with healthcare benefit plans, ensuring a comprehensive understanding of their fiscal dimensions.
Addressing Issues Related to Post-Retirement Health Plans:
Exploring the unique challenges and considerations tied to post-retirement health plans, recognizing their long-term implications.
Discussing Financial Issues Related to Healthcare Benefit Plans:
Examining the broader financial landscape surrounding healthcare benefit programs, considering budgetary implications and financial sustainability.
Explaining Tax Dimensions of Healthcare Benefit Plans:
Unraveling the tax implications inherent in healthcare benefit plans, shedding light on regulatory frameworks and considerations.
Introducing the International Financial Reporting Standards and Employee Health and Welfare Plans:
Providing insights into the global context by introducing the International Financial Reporting Standards and their relevance to employee health and welfare plans.
In essence, this chapter aims to equip readers with a holistic understanding of healthcare benefit programs, addressing not only their historical evolution and operational intricacies but also delving into critical financial, design, and regulatory dimensions that shape the landscape of employee health and welfare.
A healthcare benefit program serves as a safeguard for employees, shielding them from the financial implications of medical expenses. It operates by assessing the collective risk associated with healthcare needs, spanning from minor incidents to major emergencies within a targeted group. The primary objective is to establish a financial reservoir, ensuring the availability of funds to cover medical costs promptly as employees or their dependents encounter them.
As defined by the Health Insurance Association of America, health insurance is characterized as "coverage that provides for the payments of benefits as a result of sickness or injury." In essence, the healthcare benefit program is meticulously crafted to furnish employees and their dependents with a robust shield against potential financial setbacks arising from medical expenditures, encompassing both routine and critical healthcare requirements.
A Brief History of Healthcare Benefits
Prior to the 1930s, the onus of healthcare expenses rested squarely on the shoulders of the ailing or injured individuals and their families. However, the landscape underwent a significant shift post the Great Depression, giving rise to the inception of the inaugural Blue Cross plans. The late 1930s witnessed the integration of physicians into the equation with the establishment of Blue Shield plans. Through the 1940s, Blue Cross and Blue Shield emerged as the primary purveyors of healthcare protection plans.
While the proliferation of Health Maintenance Organization (HMO) plans is commonly attributed to the 1950s, there is compelling evidence challenging this notion, as exemplified by the initiation of Kaiser plans in the late 1920s.
Witnessing the success of Blue Cross and Blue Shield, insurance companies ventured into the realm of medical insurance. They introduced hospital coverage initially and subsequently expanded their offerings to encompass doctor charges and surgical procedures.
The advent of national health insurance marked a pivotal moment as the federal government intervened on behalf of the elderly and the impoverished. Medicare, catering to individuals over 65, was financed through a combination of government revenue, premiums from enrollees, and taxes from both employers and employees. Complementing this initiative, Medicaid was established to provide healthcare protection for low-income wage earners.
From the 1970s onward, the landscape of healthcare benefits underwent a myriad of design changes. The ensuing chapters of this book delve into the intricate details of these ever-evolving dynamics, primarily propelled by the driving force of cost considerations.
The Prevalence of Healthcare Benefit Plans
The latest census report for the year 2011, published in September 2012, provides insightful data on the prevalence of employer-sponsored healthcare plans among the total United States population of 312,250,315 citizens.
According to the report:
The number of individuals covered by health insurance saw an increase to 260.2 million (84.3%) in 2011, compared to 256.6 million (83.7%) in 2010.
The percentage of people covered by private health insurance in 2011 remained statistically unchanged from 2010, holding steady at 63.9%. This marks the first instance in the past decade where this rate has not experienced a decrease.
Employment-based health insurance coverage in 2011 remained stable at 55.1%, showing no significant change from the previous year.
Government health insurance coverage experienced a slight increase from 31.2% to 32.2%.
The percentage of individuals covered by Medicaid, the federal healthcare program for low-income families and individuals, rose from 15.8% in 2010 to 16.5% in 2011. Similarly, for Medicare, the federal healthcare program for the elderly, the percentage increased from 14.2% to 15.2%.
In 2011, 9.7% of children under the age of 19 (7.6 million) were without health insurance, a statistically unchanged figure from the 2010 estimate. Similar stability was observed for individuals aged 26 to 34 and those aged 45 to 64. However, a decline in the percentage of uninsured was noted for individuals aged 19 to 25, 35 to 44, and those aged 65 and older.
The uninsured rates in 2011 exhibited a downward trend with increasing household income, dropping from 25.4% for households with an annual income below $25,000 to 7.8% for households with an annual income of $75,000 or more.

*The presented estimate is statistically distinct from the estimate for the previous year (p<.05).
Note: As outlined in the Survey Design and Methods section, the estimates featured in this exhibit are derived from both the sample of firms that completed the entire survey and those that responded to a single question regarding the provision of health benefits.
The Structure of Healthcare Benefit Plans
The management and administration of reimbursement processes for medical expenses can be orchestrated by various entities, such as governmental agencies, private businesses, or nonprofit organizations. Healthcare financial protection, encompassing the reimbursement of incurred expenses, is often channeled through diverse avenues, including insurance companies, health maintenance organizations (HMOs), preferred provider organizations (PPOs), Blue Cross, and Blue Shield. These programs have transitioned from associations to licensed insurance offerings, a transformation explored in greater detail later in this chapter.
A company sponsoring a healthcare program may directly cover expenses on behalf of employees and their dependents through a self-insured plan. The scope of covered expenses can range from specific medical categories to comprehensive coverage encompassing all types of expenses.
Empirical evidence underscores that, among the array of functional benefits embedded in an employment contract, healthcare benefits are overwhelmingly deemed the most significant by workers. As the costs of medical care escalate, the importance of healthcare benefits to employees intensifies. This heightened significance arises from the potentially ruinous financial impact of medical costs, particularly those associated with major medical procedures, in the absence of company-sponsored healthcare benefits. Individuals often find themselves on the brink of bankruptcy when grappling with the financial burden of unexpected and catastrophic medical incidents.
Crucially, employer-sponsored healthcare benefit plans are undergoing substantive structural changes. A healthcare benefit study conducted in 2012 by the management consulting firm Oliver Wyman illuminated a major conundrum faced by companies. With the enactment of healthcare reform legislation (the Patient Care and Affordable Care Act of 2010), companies express a strong commitment to safeguarding their employees through company-sponsored healthcare programs. Simultaneously, these companies acknowledge that the long-term sustainability of providing such healthcare is in question. Employers find themselves at a crossroads, navigating a delicate balance between upholding their commitment to employee well-being and grappling with the escalating costs. The coming years will be pivotal as the tangible impact of the Affordable Care Act unfolds.
Healthcare Benefit Plan Design Considerations
The concept of healthcare benefits has undergone a transformative journey through the years. In the contemporary landscape, healthcare benefits encompass a broad spectrum, ranging from doctor charges—including associated tests and procedures—to hospitalization, dental care, and vision-related expenses. Beyond the traditional scope, healthcare benefits also extend to cover lost income, wellness-related costs, expenses related to addiction suppression, and various other facets of healthcare expenditure.
For the purposes of our discussion, we specifically define healthcare benefits as inclusive of medical expenses, dental costs, and vision-care expenditures.
The design of healthcare benefit plans is intricately shaped by a myriad of factors and features. Notably, recent decisions in plan design reflect a concerted effort to grapple with the imperative of managing escalating costs. Key considerations in this regard include:
Deductibles
Co-insurance
Copayments
Exclusions and limitations
Maximum benefits
Preadmission testing
Second surgical opinions
Coordination of benefits
These elements collectively contribute to shaping the contours of healthcare benefit plans, illustrating the dynamic interplay between evolving healthcare needs and the imperative of cost containment.
The People that Pay
In the United States, while public health insurance is a relatively recent phenomenon, the landscape of healthcare has long been dominated by private insurance entities. Commercial insurance has played a substantial role in providing healthcare benefits, with casualty and life insurance companies extending their services to encompass the healthcare sector.
Prominent examples of commercial insurance companies in this realm include Aetna, Humana, and United Health Group, typically offering group insurance coverage. Traditionally, healthcare benefits have been structured through a mechanism known as an indemnity plan, also referred to as a fee-for-service plan. Under this arrangement, employees have the flexibility to choose any medical provider, be it a doctor or hospital. Further insights into this concept are detailed in Chapter 3, "Healthcare Benefit Financing."
To enhance the integration of healthcare services and insurance, insurers have pioneered managed-care organizations. These entities, often created by insurers with their own provider networks or through contractual arrangements with other providers, seek to streamline healthcare delivery and insurance within a unified framework. The most prevalent form of managed-care organization is the health maintenance organization (HMO), whose development was incentivized by the Federal Health Maintenance Act of 1973.
This legislation facilitated the growth of HMOs by providing grants and loans for their establishment, expansion, or initiation. It also relaxed certain state restrictions for federally qualified HMOs, mandating employers with 25 or more employees to offer federally certified HMO options alongside traditional health insurance, without, however, compelling the provision of health insurance.
Fundamentally, HMOs aim to control costs and ensure effective healthcare by constraining patients to specific providers. This control is exerted through a provider panel mechanism and the involvement of primary care physicians who must authorize specialized care and referrals; bypassing this review process may result in non-payment of benefits.
While HMOs proliferated in the 1980s and 1990s, they faced declining popularity among employees due to the restrictions imposed on their healthcare choices. Responding to this shift, insurers introduced an alternative model known as a preferred provider organization (PPO). PPOs, in contrast to HMOs, do not mandate participants to use specific providers but incentivize such choices through reduced prices offered by network providers. Additionally, PPOs often do not necessitate participants to undergo primary care physician reviews, providing a more flexible approach to healthcare access.
Both Health Maintenance Organizations (HMOs) and Preferred Provider Organizations (PPOs) have spearheaded the era of managed care, representing a paradigm shift in healthcare administration. Broadly, these plans and organizations are designed to exert control over the decision-making process, aiming to effectively manage medical expenses. Five key characteristics typify these managed care arrangements:
Controlled Access to Providers:
Managed care plans regulate and manage access to healthcare providers, steering participants toward specified networks of doctors, hospitals, and other healthcare professionals.
Comprehensive Utilization Management:
These plans engage in comprehensive utilization management, scrutinizing and optimizing the use of healthcare services. This involves assessing the necessity and efficiency of medical treatments and procedures.
Encouragement of Preventive Care:
Emphasizing a proactive approach to healthcare, managed care plans actively encourage preventive care measures. Participants are often incentivized to undergo regular check-ups, screenings, and vaccinations to mitigate potential health risks.
Facilitation of Risk Sharing Among Providers:
Managed care arrangements promote a collaborative approach among healthcare providers by facilitating risk-sharing mechanisms. This involves distributing and managing financial risks among the provider community to achieve cost-effective healthcare delivery.
Ensuring Quality Healthcare Delivery:
Quality assurance is a cornerstone of managed care plans. These organizations implement measures to ensure the delivery of high-quality healthcare services, encompassing standards for medical practices, patient outcomes, and overall healthcare effectiveness.
In essence, the guiding principles of managed care, as embodied by HMOs and PPOs, seek to optimize the healthcare system by aligning incentives, promoting preventative measures, and enhancing the overall quality and efficiency of healthcare delivery.
Payment Options
Healthcare programs employ two primary payment methods: fee-for-service and capitation. Within fee-for-service programs, three distinct methods are prevalent:
Cost-Based Reimbursement:
In this method, the payer agrees to cover the costs incurred in delivering services to the insured. Cost-based reimbursement is confined to allowable costs, typically encompassing expenses directly associated with providing healthcare services.
Charge-Based Reimbursement:
Payers are billed for services based on a predetermined rate schedule. Payments are commonly made on negotiated, discounted charges. Managed-care plans, leveraging their substantial member groups, wield the bargaining power to secure these discounts, which can range from 10% to 50% or more on stated charges.
Prospective Payments:
Rates in this system are established before services are rendered and are unrelated to costs or charges. Common units of payment include per procedure, per day, or a comprehensive global reimbursement process. In the latter, a single payment covers all services associated with a particular treatment or medical intervention.
In contrast, capitation represents a distinct payment paradigm. Under capitation, providers receive a fixed amount per covered life within a specified period, typically monthly, regardless of the actual services rendered. The reimbursement is determined based on the number of participants assigned to the provider, resulting in a fixed payment structure anchored in population coverage. This approach fundamentally shifts the reimbursement model from a service-centric perspective to one grounded in the overall population served.
Consumer-Driven Healthcare
Numerous organizations are embracing an alternative approach to healthcare through the adoption of Consumer-Driven Health Plans (CDHPs). At the core of these programs is a philosophy that actively engages consumers to directly influence and contain healthcare costs. The underlying principle is rooted in the belief that individuals, armed with proper information, tools, and financial incentives, can become more discerning and responsible healthcare consumers. A CDHP, therefore, empowers consumers with a sense of personal responsibility to facilitate this shift.
Typically, a CDHP incorporates a high deductible paired with an individually controlled healthcare account, featuring either a Health Savings Account (HSA) or a Health Reimbursement Account (HRA). These intricacies are expounded upon later in this chapter. The combination of a high-deductible plan and one of these account options aims to instill and encourage responsible behavior on the part of the consumer. These plans go beyond mere coverage by providing essential information and tools that enable informed decision-making.
Key components integral to a CDHP include:
• High-Deductible Health Plan:
The cornerstone of a CDHP involves a high-deductible health plan, creating a financial threshold that encourages consumers to be judicious in their healthcare choices.
• Individual Health Account:
An individually managed health account, housing either an HSA or HRA, serves as a financial reservoir to cover expenses not met by the plan. These accounts provide a personalized approach to managing healthcare costs.
• Information and Tools:
CDHPs emphasize the provision of comprehensive information and tools to empower participants in making well-informed decisions regarding their healthcare.
• Communication Program:
A robust communication program is developed to guide participants through decision-making processes, ensuring clarity and understanding of the intricacies of the CDHP.
• Healthcare Coach or Consultant:
Access to a healthcare coach or consultant further enhances the support structure, aiding participants in navigating the complexities of healthcare choices and strategies.
• Severe Chronic Illness Management:
Specialized programs for managing severe chronic illnesses, facilitated by licensed medical practitioners, are integrated into CDHPs, demonstrating a commitment to holistic healthcare management.
In essence, CDHPs embody a paradigm that not only transforms the financial dynamics of healthcare but also seeks to foster a culture of informed decision-making and responsible consumer behavior.
It's crucial to note that consumer-driven healthcare represents a relatively recent and innovative design feature. Generally, this initiative adopts one of two approaches. The first approach is commonly referred to as a defined contribution medical expense plan. Under this model, employers offer various options such as HMOs, PPOs, or an indemnity plan. The employer's contribution is set at the level of the lowest-cost item, often the HMO plan. If employees opt for a more expensive (and typically better) option, they are required to pay a higher out-of-pocket premium, constituting a high-deductible healthcare plan (HDHP).
In this scenario, the employer contributes a portion of the deductible. For instance, if the plan's deductible is $6,000, the employer might contribute $3,000. Should the employee choose this plan, a dedicated savings account is established, into which contributions are deposited. Funds from this account can be withdrawn for medical expenses, with the flexibility to roll over unused funds to the following year.
These plans are strategically designed to incentivize wise decision-making in seeking medical care services, as any expenditures exceeding the funds in the savings account must be fully covered by the employee.
High-deductible plans present a notable reduction in the overall cost of providing healthcare benefits. Furthermore, many employers view these plans as highly effective in transforming employees into informed consumers of expensive healthcare services. Notably, since 1996, employer contributions to the savings plan have been non-taxable for employees, adding a significant financial benefit to this consumer-driven healthcare approach.
To ensure the effectiveness of such a plan, the key focus should be on educating employees about medical needs, costs, and outcomes. With both their employers' contributions and their own funds deposited into the account, employees are incentivized to make informed decisions—essentially, to shop around for the most economical and cost-effective medical services.
In the second approach to consumer-driven healthcare, employees retain control over directing their expenditures using funds they specifically set aside for these purposes. When individuals spend their own money, a strong incentive is created to be responsible when purchasing healthcare, fostering self-imposed cost-containment measures.
This second approach leverages various government-supported, tax-favored incentives and programs, including:
• HSAs (Health Savings Accounts):
These accounts allow individuals to save money tax-free for qualified medical expenses. The funds contributed to an HSA roll over from year to year, offering a long-term approach to managing healthcare costs.
• HRAs (Health Reimbursement Accounts):
HRAs provide employers with the flexibility to reimburse employees for eligible medical expenses. Unlike HSAs, HRAs are solely funded by the employer, offering a tax-advantaged benefit to employees.
• FSAs (Flexible Spending Accounts):
While not precisely classified as consumer-driven, FSAs operate as a pre tax spending provision. Employees contribute to an FSA with pretax dollars, which can be used for eligible medical expenses during the plan year.
Accounting Implications and Issues Affecting Healthcare Benefit Plans
This section delves into the intricacies of healthcare plan design, exploring the technical dimensions that span accounting, tax implications, legal considerations, financial aspects, and auditing requirements.
The Standards Framework
In the United States, the accounting of health and welfare programs is shaped by two pivotal guiding principles, as established by the generally accepted accounting principles (GAAP), the Financial Accounting Standards Board (FASB), and the Employee Retirement Security Act (ERISA). On the international front, the corresponding principle is the International Financial Reporting Standards (IFRS).
Under the U.S. GAAP, the accounting for health and welfare plans is outlined in FASB Accounting Standards Codification (ASC) Regulation 965, while IFRS codification is addressed in IAS 19.
Throughout this section, our discussion is anchored in these rules, regulations, and principles, specifically under the U.S. GAAP (FAS 965) and the IFRS (IAS 19). You will gain insights into the essential elements of accounting requirements as prescribed by these relevant codes.
Companies in the United States have been diligently examining the distinctions between the International Financial Reporting Standards (IFRS) and the U.S. Generally Accepted Accounting Principles (GAAP) in anticipation of a potential convergence of standards. The industry is on standby, awaiting any forthcoming mandates from rule-making bodies that might require U.S. companies to adopt IFRS standards.
Conducting a comprehensive analysis, interpretation, and understanding of Financial Accounting Standards Board (FASB) standards, particularly in the context of benefits accounting, is a valuable undertaking. Simultaneously, a similar analysis must be applied to IFRS standards, given the prospect of convergence in the near future.
A robust understanding of the accounting principles under both sets of standards will prove instrumental in facilitating a smooth convergence process, should it be mandated. Later in this chapter, the discussion delves into IFRS regulations related to health and welfare, offering a comprehensive exploration of these international standards.
It's important to note that the ongoing discussion is rooted in a direct analysis and comprehensive examination of these standards, providing a foundational understanding for navigating the potential convergence landscape.
Defined Contribution Versus Defined Benefit Plans
Defined contribution health and welfare plans stand apart from defined benefit plans through their distinct operational mechanisms. In a defined contribution plan, meticulous records are maintained for each participant's account, detailing contributions made by both participants and their employers. This comprehensive record-keeping extends to encompass various elements, including flexible spending arrangements, vacation plans, and Health Savings Accounts (HSAs).
Contrastingly, a defined benefit plan outlines a specific benefit, which may take the form of reimbursement to the covered participant or direct payments to providers or third-party insurers for stipulated services. Participants in defined benefit plans receive a predetermined benefit determined by a formula stipulated within the plans themselves. In contrast, defined contribution plans furnish benefits based on the cumulative amounts contributed to individual participant accounts. The key distinction lies in the method of benefit determination, with defined benefit plans specifying the outcome, while defined contribution plans derive benefits from accumulated contributions.
In the context of defined benefit plans, several components contribute to their financial dynamics, each holding inherent value. These include:
• Forfeitures:
Forfeitures represent a component that contributes to the overall value of the defined benefit plan. These are assets that were once allocated to a participant but are subsequently relinquished, typically due to factors like the participant leaving the plan before full vesting.
• Investment Experience:
The investment experience is a critical factor influencing the financial health of a defined benefit plan. It encompasses the returns and performance of the plan's investments, exerting a direct impact on the overall value and sustainability of the plan.
• Administrative Expenses:
Administrative expenses constitute a vital element in the financial makeup of defined benefit plans. These expenses cover the costs associated with managing and maintaining the plan, ensuring its smooth operation and compliance with regulatory requirements.
Given the intrinsic value associated with each of these components, the financial statements of a defined benefit plan play a pivotal role in offering insights into its current and future capacity to meet benefit obligations as they become due. To fulfill this mandate, the plan's financial statements should present comprehensive information about its assets and benefit obligations, the outcomes of transactions or events affecting its assets and liabilities, and any other pertinent details essential for stakeholders to analyze the information presented.
It is imperative that different types of defined benefit plans, whether multiemployer or single employer, distinctly report benefit obligations, encompassing those related to post-retirement scenarios. This separation aids in providing a clear and transparent representation of the plan's financial standing and commitments.
Section 965 Explained
• Benefit Payments (965-30-25-1):
Health and welfare plans manage benefit payments either directly or through the utilization of a third-party administrator (TPA) in an administrative service arrangement (ASA). Benefit payments are processed by fully or partially self-funded plans, highlighting the versatility in plan structures.
• Premiums Due Under Insurance Arrangements (965-30-25-3):
Unpaid premiums due under insurance arrangements should be integral to the accounting for any obligation. Recognizing the pending premium payments is essential for an accurate representation of the plan's financial standing.
• Post-Employment Benefits (965-30-25-3):
For post-employment benefits, a benefit obligation must be recognized for current employees based on future payment amounts, subject to specific conditions. These conditions encompass the employee's right being tied to services rendered, vested benefits, a high probability of payment, and accurate estimation. An exception exists for plans offering uniform benefits due to an event like medical benefits under a disability plan, which typically lacks a vesting provision.
Disability benefits must be accrued from the disability's onset (965-30-25-4).
• Obligations for Premium Deficits (965-30-25-5):
Fully insured experience-rated plans may incur deficits based on experience ratings determined by insurance companies. These deficits must be incorporated into the total benefit obligation if certain criteria are met, including the probability of applying the deficit against future premiums or experience-rated refunds.
• Recognition of Employer Contributions (965-310-25-1):
If an employer formally commits to contributions, documentation is imperative. Sufficient evidence may include a governing body resolution, a consistent payment pattern under a funding policy, proof of federal tax deductions, and an accounting recognition as a current liability. Mere accruals or liability amounts exceeding plan assets are deemed insufficient for recognition.
This nuanced breakdown ensures a comprehensive understanding of the various components and considerations in the accounting landscape of health and welfare plans.
• Recognition of Premiums Paid to Insurance Companies (965-310-25-2):
The recognition of premiums paid to insurance companies hinges on whether the payments serve as a transfer of risk or function as a deposit. A meticulous analysis is necessary to determine the extent of risk transfer. Insurance companies might mandate a deposit for potential losses, and these deposits are considered plan assets until applied to premiums. In cases where reserves are forfeitable upon termination of the insurance contract, this factor must be factored into asset calculations. If experience-rated premium refunds are anticipated, and if the policy year doesn't align with the plan, expected refunds should also be documented as plan assets. It is assumed that all calculations can be reasonably performed, per 965-310-25-3.
• Calculating Plan Benefit Obligations (965-30-35-1):
The calculation of benefit obligations for single/multiemployer defined health and welfare plans necessitates the inclusion of the actuarial present value of various elements:
Claims Payable:
The present value of claims that are currently payable.
Claims Incurred But Not Reported (IBNR):
The present value of claims that have been incurred but not yet reported.
Premiums Due to Insurance Companies:
Premiums due for accumulated credits and postemployment benefits. This encompasses premiums for retired participants, including beneficiaries and dependents, as well as other eligible participants and those not yet fully eligible. This crucial information should be integrated into the body of financial reports rather than relegated to footnote disclosures.
Claims Incurred But Not Reported
A crucial concept impacting both the actuarial valuations of plan assets and liabilities is IBNR (claims incurred but not reported). An IBNR claim represents healthcare services that have been provided but remain unrecorded or unprocessed by the healthcare provider, clinic, hospital, or any other health service organization. Typically, IBNRs are integral to risk-adjusted contracts between managed-care organizations and healthcare providers. In essence, an IBNR claim denotes the estimated cost of medical services for which a formal claim has not yet been filed. Efficient monitoring of these claims is typically facilitated through an IBNR collection system or control sheet. This concept plays a pivotal role in accurately assessing the financial landscape of health and welfare plans, ensuring comprehensive consideration of both reported and unreported liabilities.
In a more formal context, IBNR (claims incurred but not reported) represents the financial accounting of all services that have been performed but, due to a time element or "lag," have not been invoiced or recorded as of a specific date. The proper accounting for transactions covering provided medical services involves the following accrued but not reported IBNR entry:
• Debit—Accrued Payments to Medical Providers or Healthcare Entity
• Credit—IBNR Accrual Account
For instance, consider a scenario in a hospital where a coronary artery bypass surgery is performed for a managed care plan member. The surgeon or healthcare organization incurs expenses for related services, such as therapy, rehabilitation, drugs, and durable medical equipment, from a future payment fund. These payments constitute contractual obligations, representing a liability.
However, the health plan may not receive the complete billing until several weeks, months, or quarters later, possibly even further downstream in the reporting year post-patient discharge. To accurately project the health plan's financial liability, both the health plan and the hospital must estimate the cost of care based on historical expenses.
Given the paramount importance of identifying and controlling costs in financial healthcare management, an IBNR reserve fund (an interest-bearing account) is established for claims reflecting services already delivered but not recorded or reimbursed by a specified deadline.
From an accounting perspective, the IBNR needs to be accrued as an expense and a short-term liability for each fiscal month or accounting period. This ensures that the organization remains financially capable of fulfilling the associated claims even if the corresponding revenue has already been expended. Properly managing these "bills in the pipeline" is crucial for proactive providers and health organizations. IBNRs gain particular significance with newer patients who may present with higher medical needs than historical norms.
Amounts that hospitals anticipate recovering (recoverables) are incorporated into their reserve charges. In many instances, these recoverables may eventually transition into IBNR losses, recorded as IBNR claims on the balance sheet. As these book losses transform into actual losses, hospitals may seek reimbursement from insurers, a process that could involve disputes over the charges.
For self-funded plans, the measurement of IBNR cost is a critical process that involves assessing the present value of the plan's estimated ultimate cost for settling claims. The estimated ultimate costs should encapsulate the plan's responsibility to pay claims to or for participants, extending beyond the financial statement date if specified, and encompassing considerations such as continuing health coverage or long-term disability. This approach, outlined in 965-30-35-1A, ensures a comprehensive evaluation that reflects the plan's obligations, irrespective of participants' employment status, providing a robust foundation for financial reporting.
Other Benefit Obligations
Administrative Expenses Recognition (965-30-35-2):
Administrative expenses incurred by the plan can be appropriately recognized by either incorporating the estimated administrative expenses into the benefits expected to be paid or by adjusting the discount rate. This flexible approach, as outlined in 965-30-35-2, ensures a comprehensive reflection of administrative costs in the overall financial considerations of the plan.
Measurement of Postretirement Benefit Obligation (965-30-35-2):
The postretirement benefit obligation should be meticulously measured as the actuarial present value of future benefits linked to the participant's service performed as of the cost measurement date. The calculation, reduced by projected future contributions from plan participants, serves as the employer's funding requirement and the accumulated plan assets. Key considerations in this calculation include the continuity of the plan, the assurance that assumptions about future events will be met, accounting for anticipated forfeitures, and integration with other plans. The discount rate utilized should align with the rate of return matching high-quality fixed income investments.
Calculation of Insurance Premiums for Plan Participants (965-30-35-9):
The insurance premiums paid for plan participants who have accrued sufficient eligibility credits or hours of employment should be determined by multiplying eligibility credits by the current insurance premium. For self-funded plans, the calculation involves using the average of all benefits per eligible participant. Mortality rates, expected employee turnover, and other necessary assumptions must be factored into this calculation for accuracy.
Additional Premiums Due to Exceeding Loss Ratio (965-30-35-9):
Any additional premiums resulting from the loss ratio exceeding a specified percentage should be duly considered. This ensures that the financial impact of surpassing the expected loss ratio is appropriately reflected in the overall financial framework of the plan.
Additional Payments to Insurance Companies under Stop-Loss Arrangements (965-30-35-12):
Provision for additional payments to insurance companies arising from stop-loss arrangements is vital. This entails recognizing and accounting for any extra payments triggered by the stop-loss provisions, emphasizing the need for comprehensive financial planning and risk management.
These nuanced considerations, as delineated in the specific accounting standards, contribute to a robust financial management approach for health and welfare plans.
Additional Obligations for Postretirement Health Plans
In accounting for benefits provided as part of a postretirement health plan, the estimation of payments to participants is a crucial aspect of financial management. Typically commencing either on the retirement date or at a specified age, the calculation of the estimated obligation as of a given date relies on the actuarial present value of all future benefits attributable to the participant's period of employment. The covered individuals in benefit obligation calculations encompass:
• Retirees
• Terminated Employees (if benefits have been earned)
• Beneficiaries (or covered dependents)
• Active Employees, Their Beneficiaries, and Covered Dependents
The thoroughness of benefit obligation calculations demands consideration of the following assumptions and calculation elements:
• Appropriate Discount Rates: Reflecting the time value of money to ensure accurate present value assessment.
• Per Capita Cost of Claims by Age: Recognizing variations in healthcare costs across different age groups.
• Healthcare Cost Trends: Incorporating anticipated changes in healthcare costs over time.
• Medicare Reimbursement Rates: Considering the impact of Medicare reimbursement on overall benefit obligations.
• Retirement Age: Accounting for variations in retirement age among participants.
• Dependency Status: Differentiating benefits based on the dependency status of participants.
• Mortality: Factoring in mortality rates for precise estimations.
• Salary Progression: Accounting for changes in salary over the course of employment.
• Probability of Payment Calculation: Evaluating the likelihood of actual payment of benefits.
• Participation Rates: Considering the rates at which individuals participate in the benefit plan.
These comprehensive considerations and calculations ensure that the estimation of benefit obligations aligns with the dynamic nature of postretirement health plans and provides a solid foundation for financial reporting and planning.
Benefit obligations, as calculated for postretirement health plans, should explicitly exclude death benefits that may become payable during employees' active service periods. The determination of this benefit obligation typically involves applying current insurance premium rates or, in the case of a self-funded plan, the average cost of benefits per eligible employee. The calculation is intricately linked to assumptions regarding mortality rates and the probability of employee turnover, ensuring a comprehensive and realistic assessment of future obligations.
(Refer to 965-30-35-15 to 22 for detailed guidance on these exclusions and the calculation methodology.)
Fair Value Measurement
Fair value, within the context of healthcare benefits, is a pivotal concept that denotes "the price that would be received to sell an asset or paid to transfer a liability in an orderly transaction between market participants at the measurement date" (FASB ASC 820-10-20). This definition, provided by the Financial Accounting Standards Board (FASB) ASC 820, not only outlines fair value but also establishes a comprehensive framework for its measurement and mandates specific disclosure requirements.
To fulfill these requirements, a collaborative effort among management, custodians, investment fiduciaries, and plan auditors is indispensable. Sponsors and administrators bear the responsibility of ensuring the implementation of a robust valuation process, the availability of accurate data for fair value determination, adherence to the prescribed measuring framework, and inclusion of requisite disclosures.
A condensed overview of FASB ASC 820 is presented below:
Noncash Contributions: Contributions in noncash form must be recorded at fair value (FASB ASC 965-20-30-1). In case of a subsequent sale, the sale value is determined as the fair value minus the cost.
Financial Statements Presentation: Statements for the plan must present total assets, liabilities, net assets available for benefits, and net assets reflecting investments at fair value (FASB ASC 965-20-45-1). All associated accounting for these assets reflecting investments should ensure their presentation at fair value (FASB ASC 965-20-45-2-5).
Unusual or Infrequent Statements: Disclosures are required for unusual or infrequent events or transactions occurring after the financial statement date if they significantly impact the financial statements. A notable change in the fair value of plan assets is a mandatory disclosure event (FASB ASC 965-20-50-1).
Investments Recording: Equity, debt securities, real estate, or other investments must be recorded at their fair value as of the financial statements date (FASB ASC 965-320-35-1 / FASB ASC 965-325-35-1).
Net Appreciation or Depreciation Disclosure: The notes for financial statements must disclose the net appreciation or depreciation of the investments' fair value (FASB 965-320-50-1).
Insurance Contracts: As per the Employee Retirement Income Security Act, insurance contracts should be presented at fair value or at the amount determined by the insurance company (e.g., contract value) (FASB ASC 965-325-35-3).
In essence, compliance with FASB ASC 820 is essential for transparent and accurate reporting of fair value in healthcare benefit plans, requiring a thorough understanding and collaboration among various stakeholders to ensure effective implementation and disclosure.
Financial Statements of Defined Benefit/Contribution Plans
The primary objective of crafting a financial statement for a defined benefit health and welfare plan or a defined contribution plan is to furnish pertinent financial information for assessing the plan's current and future capacity to meet its benefit obligations in a timely manner. This necessitates the inclusion of comprehensive details about plan resources, benefit obligations, as well as transactions and events pertaining to the plan within the financial statement. Supplementary information that enhances the comprehension of this financial data may also be incorporated.
For defined benefit plans, adherence to an accrual basis of accounting is imperative. The financial statement for such a plan should encompass a statement of net assets available for the year's benefits, presenting crucial information concerning investments, insurance contracts, and investment contacts. Additionally, a statement of changes in these assets is essential, highlighting significant alterations occurring throughout the designated year.
These changes encompass:
Contributions
Fluctuations in the value of investments and associated income
Modifications in income taxes, whether paid or payable
Adjustments in payments for claims and premiums
Alterations in operating and administrative expenses
In the event of adjustments to employer contributions, a meticulous separation of cash and noncash components is imperative. Noncash contributions must be elucidated in a note outlining their nature. Further considerations concerning alterations to contributions, including those from other identified sources such as state subsidies or federal grants, need to be addressed, whether related to employees or collected and remitted. This meticulous detailing ensures a comprehensive and transparent representation of the plan's financial dynamics, fostering a more insightful evaluation of its ability to meet benefit obligations both currently and in the future.
Concerning changes in investment value, whether resulting in net depreciation or appreciation, it is imperative to address them distinctly based on the measurements of the investment's fair value. The determination of fair value involves ascertaining whether the value is derived from a quoted price in an active market or through another method.
It is crucial to note that changes in the payment for a claim exclude alterations to contracts made by the insurance company, as these are not considered part of plan assets.
The third element incorporated into the financial statement of a defined benefit plan pertains to information about the plan's obligations throughout the year.
Furthermore, the ultimate inclusion in the financial statement for a defined benefit plan encompasses details regarding the impact of changes in the plan's obligations. All factors instigating these changes over the plan's duration must be meticulously identified. This encompasses amendments, alterations in the nature of the plan, and modifications in actuarial assumptions, constituting the minimum disclosures concerning changes in benefit obligations.
Certain defined contribution plans impose balance limitations on participants' accounts, such as vacation plans, holiday plans, and legal plans (FASB ASC 965-205-10-1-2). The requisite financial information encompasses details about plan resources, their functioning, management, and the outcomes of transactions and events influencing these resources, along with other factors enhancing the comprehension of the provided information. Essential components include a statement of net assets available for plan benefits throughout the year and the statement of changes in net assets. This ensures a comprehensive and transparent representation of the plan's financial dynamics and aids in evaluating its performance and impact on participant accounts.
Self-Funding of Healthcare Benefits
A pivotal financial consideration in the realm of benefit programs revolves around the concept of self-funding. In this approach, rather than procuring a pre-packaged insurance product, an employer allocates funds directly from the company's general resources to finance an employee's plan.
The landscape of healthcare costs has witnessed a consistent upward trajectory over numerous years, prompting employers to actively explore avenues for cost mitigation. Self-insured health plans emerge as a strategic solution in this context. These plans empower companies to settle submitted claims through a dynamic pay-as-you-go system, offering a flexible and cost-effective alternative. The intricacies of self-funding will be thoroughly examined and elucidated in Chapter 3, providing a comprehensive understanding of its mechanisms and advantages in navigating the evolving landscape of employee benefit programs.
Tax Dimensions of Healthcare Plans
As outlined earlier in this chapter, the Internal Revenue Service (IRS) tax codes have introduced specific healthcare initiatives. This section delves into a detailed exploration of these initiatives.
Health Savings Accounts
Established in 2003 under the Medicare Prescription Drug Improvement and Modernization Act, Health Savings Accounts (HSAs) provide a tax-advantaged avenue for individuals covered by high-deductible health plans (HDHP) to manage funds earmarked for medical expenses. Typically associated with lower premiums but higher deductibles than traditional health plans, HDHPs are designed for specific, catastrophic health events.
According to a survey conducted by the Kaiser Family Foundation in September 2008, the adoption of Consumer-Driven Health Plans (CDHP), including both HSAs and Health Reimbursement Arrangements (HRAs), witnessed a notable increase from 4% in 2006 to 8% among covered workers. Correspondingly, approximately 10% of firms offered such plans. The majority of HSA plans appeared to be employer-sponsored, with around 25% individually set up, as corroborated by a study from America’s Health Insurance Plans (AHIP), reporting a total of 6.1 million Americans covered by HSA plans as of January 2008.
An overarching trend in HSA data reveals that contributions to these plans consistently outpace withdrawals, often nearly doubling in magnitude since their inception.
Contributions to HSAs can be made by individual members of an HSA-eligible HDHP, employers, or other parties. Employer contributions subject the plan to ERISA-qualified status, activating nondiscrimination rules unless contributions are channeled through a Section 125 plan, where such rules do not apply. Employers enjoy flexibility in distribution, allowing distinctions between full-time and part-time employees, as well as variations between individual and family participants.
Contributions, whether from an employer or employee, may occur on a pretax basis, offering the advantage of avoiding FICA and Medicare tax deductions, translating to a significant 7.65% savings for both parties, within Social Security wage base limits. In the absence of employer contributions, post-tax deposits can still be utilized to reduce gross taxable income in the subsequent year. It is imperative to note that contributions are restricted to those covered under an HSA-eligible HDHP, maintaining the integrity of the account's purpose and benefits.
Initially, the annual maximum deposit to a Health Savings Account (HSA) fell below the actual deductible or specified IRS limits. However, Congress subsequently eliminated this limit tied to the deductible and established maximum contribution limits. All contributions to an HSA, regardless of their origin, contribute to an annual maximum. Additionally, a catch-up provision exists for participants aged 55 and over, allowing an increased IRS limit.
Notably, all deposits to an HSA become the sole property of the policyholder, irrespective of their source. Unwithdrawn funds roll over from year to year, providing a sustained financial reservoir. In the event that a policyholder discontinues their HSA-eligible insurance coverage, further deposits are prohibited; however, existing funds in the HSA remain accessible for use.
The Tax Relief and Health Care Act, enacted on December 20, 2006, introduced a significant provision permitting a one-time rollover of Individual Retirement Account (IRA) assets to fund up to a year's maximum HSA contribution. State tax treatment of HSAs exhibits variability.
According to IRS Publication 969: Health Savings and Other Tax-Favored Health Plans, an individual can generally make HSA contributions for a given tax year until the deadline for filing returns, typically on April 15.
For the years 2012 and 2013, the IRS stipulated contributions as follows:

Funds within a Health Savings Account (HSA) can be strategically invested, employing a methodology akin to Individual Retirement Accounts (IRAs). Notably, investment earnings enjoy tax-sheltered status until the moment of withdrawal.
While HSA funds are transferrable to other HSAs, it's crucial to note that rollovers into an IRA or a 401(k) are not permissible. Similarly, funds from IRAs and alternative investments cannot be seamlessly rolled into an HSA, with the exception of the previously mentioned one-time IRA transfer.
In a departure from some employer contributions to plans like a 401(k), all contributions to an HSA immediately become the property of the participant, irrespective of their origin. Unlike certain other accounts, HSA participants are not obligated to secure advance approval from their trustee or medical insurer to withdraw funds. Importantly, funds used for qualified expenses, encompassing services and items covered by the health plan subject to cost-sharing such as deductibles and co-insurance, remain exempt from income tax. Withdrawals can also be made for expenses beyond medical plans coverage, including dental, vision, chiropractic care, medical equipment like eyeglasses and hearing aids, and transportation expenses related to medical care. Until December 31, 2010, even nonprescription over-the-counter medications were eligible for HSA funds.
However, the landscape changed on January 1, 2011, with the implementation of the Patient Protection and Affordable Care Act, commonly known as Healthcare Reform. This legislation stipulates that HSA funds can no longer be utilized to purchase over-the-counter drugs without a doctor's prescription, highlighting the evolving regulatory environment surrounding HSA usage.
Health Savings Account (HSA) funds offer flexibility in withdrawal methods, allowing account holders to access funds through various means such as debit cards or personal checks. Withdrawals can be initiated for any reason, but it's crucial to note that withdrawals not allocated to documented and qualified medical expenses are subject to income tax and a 20% penalty. This penalty is exempt for individuals aged 65 or older or those with disabilities at the time of withdrawal. In such cases, only income tax is applicable, effectively rendering the account tax-deferred, similar to an Individual Retirement Account (IRA), with medical expenses continuing to enjoy tax-free status. Post-January 1, 2011, the penalty for nonqualified withdrawals, under the Patient Protection and Affordable Care Act, reduced to 10%.
To substantiate withdrawals, account holders must maintain proper documentation for their medical expenses. Neglecting this requirement may lead the IRS to classify expenses as unqualified, exposing the taxpayer to additional penalties.
An HSA plan represents an innovative approach designed primarily to mitigate healthcare costs for employers, thereby enhancing the efficiency of the healthcare system. The underlying principle is grounded in the belief that when individuals utilize their own funds, it fosters a sense of responsibility in healthcare decision-making, promoting cost-effective choices. Additionally, the model anticipates that individuals bearing their expenses will be more discerning in gathering information, actively seek lower-cost options, and remain vigilant against excess and fraud. Consequently, the HSA program serves as a valuable tool for containing costs in the healthcare sector.
Within the realm of Consumer-Driven Health Plans (CDHPs), two alternative plans share common objectives yet feature distinct structures: Health Reimbursement Arrangements (HRAs) and Flexible Spending Accounts (FSAs).
Health Reimbursement Accounts
Health Reimbursement Accounts (HRAs), also known as health reimbursement arrangements, are IRS-approved programs that empower employers to earmark funds for reimbursing medical expenses incurred by employees. These programs present tax advantages for both employees and employers.
Offered to both employees and retirees, this account enables participants to utilize the allocated funds for various medical expenses, including deductibles, co-insurance, and covered medical costs. Similar to Health Savings Accounts (HSAs), any unspent funds can be carried over from one year to the next, as long as the individual remains a member of the plan. Importantly, these contributions by the employer do not count as income, resulting in significant tax savings.
Employers establish and manage HRA programs, often leveraging third-party administrators. The flexibility of these plans allows participants to potentially roll over plan balances, with the employee deciding the rollover amount, either as a percentage or a fixed amount. According to IRS guidelines, HRAs must be exclusively funded by employers, and contributions cannot be facilitated through a voluntary salary reduction agreement. Notably, there is no cap on employer contributions, as these contributions are excluded from an employee's income.
As outlined in IRS Publication 96, participants in HRA programs are reimbursed tax-free for qualified medical expenses up to a maximum dollar amount for a defined coverage period. HRAs specifically reimburse items agreed upon by the employer, such as copays, co-insurance, deductibles, and services not covered by the company's standard insurance plan. Employers fund individual reimbursement accounts for their employees within the HRA framework and define the eligible uses of these funds.
Before a plan can be put into effect, qualified claims must be clearly outlined in a comprehensive plan document. Approved reimbursements may cover a spectrum of services, including medical and dental services, copays, co-insurance, and deductibles, although the specifics can vary from one plan to another. Importantly, employers are not obligated to prepay into a fund for reimbursements; instead, they have the flexibility to reimburse employee claims as they arise.
Reimbursements under an Health Reimbursement Account (HRA) plan extend to a broad scope, encompassing current and former employees, spouses, and any individual the employee may have claimed as a dependent on their tax return, with specific exceptions outlined in the plan.
A significant advantage of a plan like this lies in its ability to provide employers with predictability in their healthcare benefit expenses. This predictability contributes to effective cost containment, offering employers a clearer understanding and control over their healthcare-related expenditures for employees.
Flexible Spending Accounts
As mentioned earlier, Flexible Spending Accounts (FSAs) are not typically utilized as a cost-containment tool for employers. Instead, an FSA serves as a program designed to empower employees to efficiently allocate their own funds toward healthcare and dependent care expenses. In this arrangement, individuals can earmark a specific portion of their earnings to cover these expenses, and these funds are exempt from payroll taxes. However, a significant drawback of FSAs is that any unspent funds at the end of the year are forfeited, distinguishing them from Health Savings Account (HSA) funds, which can carry over.
The most prevalent type of FSA is designated for medical expenses. While HSAs and FSAs share similarities, the primary distinction lies in the fact that an HSA is a component of a consumer-driven plan, whereas an FSA can be integrated with either a consumer-driven plan or a traditional healthcare benefit plan. An FSA may comprise two components: one dedicated to qualified medical expenses and the other geared towards dependent care expenses.
Medical Expense FSA
The most prevalent form of Flexible Spending Account (FSA) is designed to cover medical expenses not covered by insurance, including deductibles, copayments, and co-insurance amounts. As of January 1, 2011, changes in regulations stipulated that over-the-counter medications are allowable only when acquired with a doctor's prescription, with insulin being the sole exception. Nevertheless, over-the-counter medical devices like bandages, crutches, and eyeglass repair kits remain permissible.
Prior to the implementation of the Patient Protection and Affordable Care Act, employers had the flexibility to establish any maximum for their employees. However, the enactment of this act brought about a modification in Section 125, restricting FSAs by capping employees' annual elections. This limit, set by the IRS, was initially established at $2,500 for the first plan year commencing after December 31, 2012. Subsequent plan years' limits are subject to adjustments based on cost-of-living considerations. Employers have the option to further limit their employees' annual elections. It is essential to note that this limit applies individually to each employee, regardless of marital status or dependents. Contributions not deducted from an employee's wages are not factored into this limit. In scenarios where an individual is employed by multiple unrelated employers, they are permitted to choose an amount up to the limit under each employer's separate plan. Importantly, this limit does not extend to Health Savings Accounts (HSAs), reimbursement arrangements, or the employee's share of the cost of employer-sponsored coverage.
Dependent Care FSA
Flexible Spending Accounts (FSAs) can also be established to cover expenses for an employee's dependents. Specifically, the dependent care FSA is subject to a federal cap of $5,000 annually per household. Married spouses have the option to each elect a separate FSA, but the combined total of their elections cannot exceed $5,000. Withdrawals surpassing the $5,000 threshold are subject to taxation.
In recent years, the introduction of the FSA debit card has streamlined direct access to the account for employees. This innovation has not only enhanced convenience but has also simplified the substantiation requirement, alleviating the need for labor-intensive claims processing.
However, a notable drawback of this system is that funds set aside must be utilized "within the coverage period," as defined by the specific coverage's parameters. Typically, this period aligns with the plan year, often designated as the calendar year. Any funds remaining unspent at the conclusion of this coverage period are forfeited.
These forfeited funds can be directed towards administrative costs or evenly distributed as taxable income among all participants. The coverage period concludes upon termination of employment, regardless of the initiator of this termination. The only exception to this rule is if the employee continues coverage with the company under COBRA or another stipulated arrangement.
International Financial Reporting Standards and Employee Health and Welfare Plans
Under the International Financial Reporting Standards (IFRS), accounting for employee benefits is governed by IAS 19. In this context, we focus on provisions related specifically to benefit items. It's important to note that IAS 19 also encompasses items termed employee compensation for the purposes of this discussion. Key provisions of IAS 19 within this domain include:
Short-term Benefits: These pertain to benefits payable within one year, contingent upon the employee providing the requisite services. This category covers medical benefits, vacation, and sick pay in the context of employee benefits. IAS 19 mandates that the undiscounted amount of these benefits is expected to be paid after the services have been rendered.
Post-employment Benefits: These are payable after the employment term concludes and encompass pensions, retiree health benefits, life insurance, and the continuation of medical and life benefits post-employment. This category excludes termination benefits. For defined contribution plans, IAS 19 stipulates that the recognized costs in the period are the contributions made in exchange for employee services during that period. In the case of defined benefit plans, the amount recognized in the balance sheet must equal the present value of the defined benefit obligation, adjusted for unrecognized actuarial gains or losses. Additionally, it includes unrecognized past service costs for pension plans. The balance is offset by the fair value of plan assets at the balance sheet's creation date.
Termination Benefits: These are payments made upon involuntary termination or voluntary termination where compensation has been granted for a temporary period. IAS 19 specifies that payable amounts should be recognized after the company decides to terminate an employee (or group of employees) before retirement or provide termination benefits due to an offer encouraging voluntary terminations.
IAS 19 necessitates that a company demonstrates planned termination within the terms of a formal, written plan, with no intention of canceling the plan post-termination. The standard also permits the discounting of action costs from the balance sheet after 12 months have elapsed, provided benefits are actively being paid.
Summary
This chapter delves into various aspects of healthcare benefit plans, offering insights into their historical evolution and shedding light on the contemporary changes propelled by shifts in healthcare policies. Employers' sponsored healthcare benefit plans are undergoing fundamental structural transformations, and the chapter addresses these changes while exploring crucial considerations in plan design, particularly emphasizing the pivotal factor of cost containment.
A notable addition to the landscape of healthcare benefit plans is the concept of consumer-driven healthcare, a relatively novel aspect discussed in the chapter. Two key consumer-driven approaches, namely defined contribution medical expense plans and consumer-driven healthcare plans, are thoroughly examined.
On the accounting front, the chapter elucidates the significance of ASC regulation 965 as the primary accounting rule governing healthcare plans in the United States, offering a succinct overview of the ASC 965 rules. On the global stage, the major international accounting rule for healthcare plans, IAS 19, is also outlined.
Self-funding emerges as a major financial consideration in healthcare plans, and the chapter provides a comprehensive example to elucidate the intricacies of self-funding a health plan.
Tax dimensions related to healthcare plans are also explored, with a focus on IRS tax code initiatives that introduce tax-favored healthcare options, including health savings accounts, health reimbursement accounts/arrangements, and flexible spending accounts.
In conclusion, the chapter encapsulates the International Financial Reporting Standards relevant to healthcare plans, providing a holistic perspective on the multifaceted dimensions of healthcare benefit programs.
Key Concepts in This Chapter
• Healthcare benefits
• Health maintenance organization (HMO)
• Preferred provider organizations (PPOs)
• Patient Care and Affordable Care Act 2010
• High-deductible healthcare plan (HDHP)
• Employee Retirement Security Act (ERISA)
• FASB ASC regulation 965
• IFRS codification IAS 19
• Defined contribution plans and defined benefit plans
• Claims incurred but not reported (IBNR)
• Health saving accounts (HSAs)
• Health reimbursement accounts (HRAs)
• Flexible spending accounts (FSAs)
Chapter 3 Healthcare Benefit Financing
Chapter Objectives:
Examine Healthcare Financing Challenges: Unpack the challenges inherent in healthcare financing, addressing the complex landscape influenced by factors such as escalating costs.
Explore Financing Approaches: Discuss various financing approaches employed in healthcare plans, providing insights into the diverse mechanisms used for fund allocation.
Understand ERISA and Self-Funded Plans: Elaborate on the intricate relationship between the Employee Retirement Income Security Act (ERISA) and self-funded healthcare plans, highlighting their interplay.
Illustrate with a Self-Funded Plan Example: Provide a comprehensive example elucidating the intricacies of a self-funded healthcare plan, offering practical insights.
Introduce Utilization Review: Explain the concept of utilization review, shedding light on its significance and role in healthcare financing.
Explore Value-Based Benefit Design: Introduce the concept of value-based benefit design, exploring innovative approaches that prioritize value in healthcare plans.
Concluding Thoughts on Healthcare Plan Financing: Summarize key insights and perspectives on healthcare plan financing, offering a reflective conclusion to the chapter.
Introduction:
Healthcare finance, encompassing the allocation and mechanisms of fund disbursement, is a critical aspect of the evolving landscape of employee healthcare benefits. This chapter delves into the transformative impact of escalating costs on healthcare benefit design, addressing the challenges faced in healthcare financing. The magnitude of these challenges is underscored by key data points:
In 2012, health spending in the U.S. reached an estimated $2.8 trillion, with a modest overall growth rate. The preceding year, 2011, witnessed expenditures of $2.7 trillion, reflecting a growth rate of 3.9 percent—only marginally higher than the 2009 rate. These figures, presented in a federal actuary analysis, highlight the substantial financial footprint of healthcare, averaging $8,680 per person in 2011. The healthcare sector constituted 17.9 percent of the gross domestic product in both 2010 and 2011. The chapter aims to dissect and address the complexities arising from such financial dynamics in the healthcare landscape.
Key Areas of Spending Growth (2011 over 2010):
Physician and Clinical Services Spending (4.3%): Accelerated growth from 3.1% in 2010, driven by increased utilization and complexity of services, outweighing slower price growth.
Medicare Spending (6.2%): Marked increase from 4.3% in 2010, attributed to a one-time surge in spending for skilled nursing facilities and faster growth in physician services and Medicare Advantage spending.
Private Health Insurance (3.8%): Accelerated from 3.4% in 2010, primarily due to a 0.5% increase in private health insurance enrollment in 2011, following consecutive declines from 2008 to 2010.
Retail Prescription Drugs Spending (2.9%): Growth picked up from 0.4% in 2010, influenced by price hikes in brand-name and specialty drugs, although still notably lower than the 2009 figure of 5% growth.
Out-of-Pocket Spending (2.8%): Increased from 2.1% in 2010, driven by higher cost-sharing and a rise in enrollment in consumer-directed health plans.
Areas of Slowed Spending Growth (2011 from 2010):
Medicaid Expenditures (2.5%): Growth decelerated from 5.9% in 2010, impacted by economic pressures on state budgets, a shift in spending share from federal to state governments, and slower enrollment growth.
Hospital Spending (4.3%): Slowed from 4.9% in 2010, attributed to reduced growth in hospital prices, lower utilization of hospital services, and restrained Medicaid spending on hospital care.
While these statistics are dated, they illuminate persistent trends that remain concerning. Throughout this chapter, we'll delve into the factors contributing to these trends and explore both micro and macro strategies to address the ongoing challenge of escalating healthcare costs.
Financing Approaches to Healthcare Programs
Financing Healthcare Programs: Insurance-Based and Self-Insured (Self-Funding)
Organizations navigate two primary avenues for financing their employees' healthcare programs: Insurance-Based Financing and Self-Insured (Self-Funding) approaches.
Insurance-Based Financing:
This prevalent method of financing healthcare programs encompasses four key characteristics:
Pooling of Losses: Spread losses across a group, allowing each employee to pay an average loss rather than the total incurred. This promotes cost sharing and accurate loss predictions with a large sample.
Payments for Random Losses: Insurance operates on the premise that payments are made for unforeseen, random losses.
Risk Transfer: The risk of payment is shifted from the insured to the insurer, who absorbs the risk by collecting premiums.
Indemnification: The insurer compensates the insured, wholly or partially, for expenses arising from illness or injury.
Insurance providers grapple with challenges such as adverse selection (high-risk individuals submitting claims) and moral hazard (employees incurring unnecessary expenses when someone else foots the bill). To counter adverse selection, insurers may charge higher premiums for high-risk employees, known as an underwriting provision. Moral hazard is mitigated through cost-sharing mechanisms like copays, co-insurance, and deductibles.
Traditionally, in a full health plan, the company pays a fixed premium, adjusted only if the number of enrollees increases during the year. The insurer collects premiums, and claims are paid based on policy benefits. Employees may face deductibles or copayments, and insurers often cover a percentage of the customary charge for medical services (co-insurance). Indemnity or fee-for-service plans allow employees to use any provider, with insurers reimbursing a percentage of medical expenses after the deductible is met.
Key components include:
Deductibles: Initial amount paid by the employee before insurer contributions.
Co-insurance: The percentage split between insurer and employee after the deductible.
Out-of-Pocket Maximum: A cap after which covered benefits are fully paid by the insurer.
Lifetime Limits: Ceilings on total benefits paid under the policy.
Experts recommend policies with reasonable lifetime limits, often set at $1 million or more, to ensure adequate coverage.
Self-Insured (Self-Funding):
In contrast to insurance-based financing, the self-insured or self-funding approach involves organizations directly funding their employees' healthcare plans from their general resources. Key features of self-insured plans include:
Direct Funding by Employer: Instead of purchasing insurance, the employer funds the employee's plan directly from company resources.
Flexibility and Control: Self-funding offers greater flexibility and control over plan design, allowing customization based on the organization's unique needs.
Reduced Administrative Costs: By handling claims and administration internally or through third-party administrators (TPAs), organizations may reduce administrative costs associated with traditional insurance.
Cash Flow Benefits: Employers pay claims as they arise, offering potential cash flow benefits compared to prepaying fixed premiums.
Risk Retention: Unlike insurance, where risk is transferred to the insurer, self-insured plans retain the financial risk associated with employee healthcare expenses.
Stop-Loss Insurance: Employers often purchase stop-loss insurance to mitigate the financial risk of catastrophic claims, setting a threshold beyond which the insurer covers costs.
Self-funding is particularly attractive to larger organizations with stable employee populations and financial capacity. It provides the flexibility to design plans tailored to employee needs, potentially resulting in cost savings and increased efficiency. However, the approach also involves assuming greater financial risk, especially without adequate stop-loss coverage. Employers must carefully weigh the benefits and risks before opting for self-insurance.
Utilization Review and Value-Based Benefit Design:
Two important concepts in healthcare financing are Utilization Review and Value-Based Benefit Design.
Utilization Review:
Utilization review involves assessing the appropriateness and necessity of healthcare services to ensure efficient resource utilization. It includes evaluating the medical necessity, quality, and cost-effectiveness of provided services. By scrutinizing healthcare utilization, organizations aim to optimize resource allocation, control costs, and enhance the quality of care. Utilization review processes may be conducted internally or outsourced to specialized entities.
Value-Based Benefit Design:
Value-based benefit design focuses on aligning healthcare benefits with the value derived from healthcare services. It emphasizes promoting cost-effective care and positive health outcomes. In contrast to traditional benefit designs, which may have uniform cost-sharing arrangements, value-based benefit design considers the value of specific services in achieving health goals. This approach often involves tailoring cost-sharing structures to encourage the use of high-value, preventive, or essential services while discouraging unnecessary or less effective interventions.
Healthcare financing poses significant challenges due to escalating costs. Organizations must choose between insurance-based financing, with risk transfer and cost-sharing mechanisms, and self-insured approaches, providing flexibility but involving greater financial risk. Utilization review and value-based benefit design offer strategies to optimize resource utilization, control costs, and enhance the value of healthcare services. Understanding these concepts is crucial for organizations striving to strike a balance between providing comprehensive healthcare benefits and managing financial sustainability.
Self-Insurance or Self-Funding
Expanding upon the discussion initiated in Chapter 2, titled "Healthcare Benefits," a critical financial consideration in the realm of healthcare benefits revolves around the prospect of self-funding these plans. Unlike the conventional approach of purchasing insurance products from external providers, self-funding involves an employer allocating funds from the company's general pool to finance an employee's healthcare plan. This strategic move gains significance in the context of the escalating healthcare costs spotlighted in earlier sections of this book, prompting employers to explore avenues for cost management and enhanced corporate profitability. The adoption of self-funded health plans emerges as a compelling opportunity in this pursuit.
Under the self-funding model, claims are processed through a pay-as-you-go mechanism. In essence, the employer disburses payments for each claim submitted by employees upon receipt. Alternatively, an employer may proactively earmark resources specifically for self-funded plans. In this scenario, when claims are submitted and subsequently evaluated for eligibility, the allocated resources are utilized to fulfill these financial obligations.
It is crucial to note that, despite potential misconceptions, a self-funded healthcare plan does not involve any traditional insurance components. In contrast to insured plans where an external insurer settles employee claims, and the company pays premiums to the insurance provider, self-funded plans operate outside this conventional insurance framework. The absence of an intermediary insurer alters the dynamics, offering a more direct and potentially cost-effective management of healthcare expenses.
A salient observation pertains to the distinction in cost dynamics, particularly given the substantial surge in medical premiums, surpassing other market items in the consumer price index. This phenomenon underscores the financial strain faced by companies and further underscores the strategic appeal of self-funding in mitigating such economic pressures.
Additionally, companies often engage third-party administrators on an annual fee basis to handle the intricate process of claims management for their self-insured plans. This outsourcing is driven by the recognition that the meticulous processing of these claims demands a significant investment of time and resources. By delegating this responsibility to specialized administrators, companies can navigate the complexities efficiently, optimizing their focus on core business operations.
In summary, the landscape of healthcare benefits is evolving, and self-funding emerges as a viable avenue for companies to proactively manage escalating costs, enhance financial resilience, and streamline the administration of employee healthcare plans.
ERISA and Self-Funding
The growth trajectory of self-funded healthcare plans has been significantly propelled by the enactment of the Employee Retirement Income Security Act, commonly referred to as ERISA. This comprehensive legislation casts its regulatory umbrella over all benefit plans sponsored by employers for their workforce, encompassing both pension and welfare plans. Within the ambit of welfare plans, which encompass nonpension benefits such as health, life insurance, and disability plans, ERISA places a focal emphasis on pensions.
Critical to the landscape of healthcare benefits within ERISA is Section 514, recognized as the preemption clause. This clause unequivocally asserts that "the provisions of this title and Title 4 shall supersede any and all state laws insofar as they now and hereafter relate to any employee benefit plan." Consequently, under Section 514, private-sector health plans provided by employers fall within the purview of ERISA, thereby enjoying exemption from state regulations by virtue of the quoted clause. This exemption extends to self-insured plans, shielding them from state-mandated benefits and relieving them of the obligation to pay premium taxes, given that, in the eyes of the law, employers administering such plans are not classified as insurance entities.
It is noteworthy, however, that while ERISA precludes state interference in the realm of self-insured plans, it does not impede states from regulating health plans tethered to insurance contracts. This nuanced distinction serves as an additional incentive for companies to opt for the self-funding route.
Companies strategically opt for self-funded healthcare plans to sidestep the regulatory landscape imposed by states, concurrently embracing the risks typically borne by insurance companies. This approach is particularly attractive to sizable corporations endowed with extensive resources, as it affords them the autonomy to retain capital rather than navigating the intricacies of insurance partnerships. Moreover, for entities boasting a substantial workforce, the predictability of claims from year to year establishes a stable foundation, allowing them to assume financial risks associated with self-funding in a relatively secure environment.
In essence, the interplay between ERISA regulations and the strategic advantages offered by self-funding presents an appealing option for companies seeking to tailor their healthcare plans to their unique financial and operational landscapes.
Funding of Self-insured Plans
Two distinct avenues have been highlighted for the structuring of such healthcare plans: the allocation of dedicated funds for claim payments or the adoption of a pay-as-you-go approach, where claims are settled as they are received. However, the landscape of possibilities expands further with the integration of hybrid options, where self-funding remains a central feature.
In certain scenarios, employers may opt for a nuanced approach by selectively outsourcing specific components of the comprehensive healthcare plan. This involves acquiring an insurance contract to cover only designated elements, granting the flexibility for the remaining aspects of the plan to be self-funded. Typically, these insured elements revolve around mental health or prescription coverage, and the regulatory oversight of such components lies within the purview of state governments, particularly in the states where the benefits are dispensed.
Introducing yet another dimension to the financing matrix is the mechanism of stop-loss coverage. This financial safeguard is commonly employed to mitigate the impact of catastrophic losses. Broadly categorized into two types, individual and aggregate, stop-loss coverage serves as a risk management tool:
Individual Stop-Loss Coverage: This form of coverage acts as a bulwark against the risk that a single claim will surpass a predetermined threshold. By safeguarding against such singular high-value claims, employers can navigate financial volatility associated with individual catastrophic events.
Aggregate Stop-Loss Coverage: In contrast, aggregate stop-loss coverage extends its protective mantle over the entirety of the plan, shielding against the cumulative losses of the entire pool exceeding a predefined threshold. This strategic layer of protection ensures that, in the face of a series of adverse events impacting the collective plan, financial stability is maintained.
The dynamic interplay of these funding mechanisms and risk management strategies underscores the intricate decision-making landscape for employers navigating the intricacies of healthcare plan design. The adoption of hybrid models and the strategic application of insurance contracts and stop-loss coverage offer a spectrum of options, enabling companies to tailor their healthcare benefits in a manner that aligns with their risk tolerance and financial objectives.
Prevalence of Self-insured Plans
In their 2012 annual report on Employer Health Benefits, the Kaiser Family Foundation and the Health Research and Educational Trust presented the data elucidated in the table below:
Overview of the Healthcare Plan Accounting Process
Bagan Inc. operates a self-funded healthcare plan under the administration of Anthem Health Plans, Inc., complemented by a pharmacy plan managed by Delta Dental. The healthcare coverage spans deluxe, standard, and economy levels, providing a range of options to cater to diverse employee needs. Additionally, employees have the flexibility to opt out of coverage by presenting evidence of alternative insurance arrangements.
The financial and operational facets of the health plan are synchronized with the fiscal year. Expenditures encompass medical, dental, and pharmaceutical claims, coupled with vision plan insurance premiums. To streamline the intricate process of claims management, administrative fees are remitted to a third-party administrator.
Financial sustenance for the healthcare plan emanates from both the company and its employees, fostering a collaborative approach to fund the comprehensive coverage provided. This balanced contribution model ensures the viability and sustainability of the self-funded healthcare plan, aligning financial responsibilities between the employer and the workforce.
Projection of Plan Costs and Funding Needed
The plan adopts a prospective accounting approach, strategically projecting expenditures prior to the commencement of the plan year. This forward-looking assessment serves as the foundational framework for determining the requisite funding levels from both the company and its employees throughout the ensuing plan year. The company commits a predetermined fixed dollar amount, coupled with a specified contribution per eligible employee, a determination typically made in advance of the fiscal year's inception.
The overarching objective is to establish a financial equilibrium whereby the company shoulders 80% of the net annual healthcare costs, with the remaining 20% allocated as the responsibility of the employees. This proactive financial planning ensures a structured and transparent distribution of healthcare funding responsibilities, aligning with the company's commitment to subsidize a significant portion of the overall healthcare expenses for its workforce.
Setting of Employee Charges
Employee rates are meticulously determined in advance of each plan year, taking into account a comprehensive array of factors. These considerations include:
Projected Net Costs: A thorough analysis of anticipated net costs lays the groundwork for establishing employee rates. This involves a forward-looking assessment of the expected financial outlay for the healthcare plans.
Allocated Company Funding: The commitment of financial support from the company is a pivotal factor influencing rate decisions. The company's allocated funding plays a crucial role in shaping the overall structure of employee contribution rates.
Projected Number of Employees: Anticipating the number of employees to be covered during the upcoming plan year is a key parameter. This projection contributes to the formulation of rates that align with the scale of coverage.
Projected Enrollment in Plan Options: The expected enrollment figures in each available plan option—be it deluxe, standard, or opt-out—directly influence the rate-setting process. This ensures rates are tailored to the diverse choices made by employees.
In addition to these foundational factors, other pertinent considerations come into play:
Health Plans Over- or Under-Recoveries: Learnings from previous years, whether in the form of over-recoveries or under-recoveries, contribute valuable insights to rate decisions. This allows for a nuanced approach, accounting for historical financial trends.
Stability of Employees' Rates: Prioritizing rate stability for employees is a significant consideration. Striking a balance that minimizes fluctuations in rates fosters predictability and financial security for the workforce.
Industry Average Comparisons: Benchmarking rates against industry averages is a strategic practice. This ensures that the company's rates remain competitive and reflective of broader market trends.
Maintaining Rate Structure Integrity: Preserving the integrity of the rate structure across different plan options is essential. This consideration guarantees a coherent and fair distribution of rates within the various available plans.
Taken together, these multifaceted considerations culminate in the establishment of employee rates that are not only reflective of the company's financial landscape but also attuned to the dynamic needs of the workforce and industry benchmarks.
Actual Costs and Funding Received
Throughout each plan year, Bagan Inc. incurs costs in tandem with the utilization of the healthcare plan. The financial support, as dictated by pre-established rates, is collaboratively provided by both Bagan Inc. and its employees. In the event that the accrued costs surpass the available funds allocated for that specific year, the company demonstrates its commitment to the well-being of its workforce by promptly injecting additional funding into the plan, without imposing any supplementary interest charges. Subsequently, a meticulous account reconciliation process is undertaken to rectify any disparities and restore the balance of payments, ensuring the sustained and seamless operation of the healthcare plan. This proactive and transparent approach underscores Bagan Inc.'s dedication to the financial health and stability of its comprehensive employee benefits program.
Healthcare Plan Balance (Over/Under-Recoveries)
Upon the conclusion of the plan year, a meticulous accounting process ensues, capturing the actual costs incurred by the healthcare plan. Concurrently, the designated funding is received. Should the actual costs surpass the allocated funding, this scenario is termed an under-recovery, as discussed earlier. In such instances, the plan is promptly supplemented to cover the deficit.
Conversely, if the funding exceeds the actual costs, this results in an over-recovery. Primarily, this surplus is utilized to offset any under-recovery from prior years. Any remaining balance is carried forward into subsequent periods, strategically earmarked to cushion against prospective costs and ensure a measured and equitable distribution of charges among employees. Notably, when a health plan experiences an over-recovery, no interest accrues.
Given that plan rates are established based on projections, there is an inherent variability in actual healthcare costs each year, leading to either an over- or under-recovery. Despite conscientious efforts to make accurate projections, the dynamic nature of healthcare costs introduces inherent variability. Nevertheless, both company contributions and amounts collected from employees are consistently directed toward covering plan costs, even if not expressly for the current year. This steadfast commitment ensures that the financial integrity of the healthcare plan is upheld, fostering stability and reliability for employees.
Communicating on Healthcare Accounting and Balance
Bagan Inc.'s Human Resources department is dedicated to maintaining transparent communication with employees, regularly presenting and reporting on healthcare costs and funding throughout the year. The dissemination of timely and updated information encompasses not only the intricacies of healthcare costs but also illuminates the company's accounting practices. Recognizing the significance of keeping employees well-informed, Bagan Inc. acknowledges that an informed workforce is an asset, fostering a collective understanding of the healthcare plan.
This commitment to transparency extends beyond a mere reporting obligation; it is rooted in the understanding that well-informed employees can provide valuable feedback. By equipping the workforce with comprehensive insights into healthcare plan dynamics, Bagan Inc. creates an environment where employees can actively engage with the healthcare benefits, offer constructive input, and contribute to the ongoing improvement and refinement of the company's healthcare offerings. This mutual exchange of information not only enhances employee satisfaction but also fortifies the collaborative relationship between the company and its workforce.
Healthcare Cost Containment
Over the last four decades, healthcare expenses have exhibited inflation rates approximately twice as high as those in the average consumer price index. This upward trajectory can be attributed to a myriad of factors, with some widely acknowledged as primary catalysts:
Aging Population: The global demographic shift towards an aging population has significantly driven up healthcare expenses. With age, the demand for medical care increases, and estimates indicate that the last two years of life incur higher healthcare expenses than any other period. As people live longer, the prevalence of older individuals grows, contributing to unprecedented rises in healthcare costs.
Technological Advancements: The rapid expansion of medical technology over the past 25 years has become a substantial contributor. While technology-based medical treatments are now commonplace, the associated procedures are often costly, adding to the overall escalation of healthcare expenditures.
Generous Healthcare Benefit Plans: Many employer-provided healthcare benefit plans have historically been generous in their coverage, offering first-dollar benefit coverage. This comprehensive coverage has been utilized liberally, irrespective of necessity, as there has been little incentive to avoid expensive care.
Emergence of New Diseases: The past two decades have seen a surge in new and uncommon diseases, exemplified initially by the spread of AIDS. Addressing these diseases necessitates substantial research and development costs, coupled with high treatment expenses.
Litigious Environment: The litigious nature of society has resulted in a surge of malpractice lawsuits against doctors and hospitals. To shield themselves, healthcare professionals have resorted to high-premium malpractice insurance policies, consequently inflating the costs of medical services.
Pharmaceutical Developments: The continuous evolution of pharmaceuticals has introduced a plethora of new drugs, typically accompanied by high costs, which are often passed on to consumers.
Underinsured and Uninsured Individuals: The increasing number of underinsured and uninsured individuals indirectly contributes to rising medical costs. To compensate, hospitals, doctors, and insurance companies transfer these costs to paying employees. The Patient Protection and Affordable Care Act seeks to address this issue.
Efforts to control these escalating costs have garnered attention from both corporate executives and national policymakers. National policies have undergone adjustments in the tax code to mitigate these challenges. Corporations, on the other hand, have implemented various programs, with utilization reviews being a direct and tangible strategy used to curb costs. This multifaceted approach reflects a concerted effort to grapple with the complexities of rising healthcare expenses.
Utilization Reviews
The utilization review process, a longstanding practice, serves to assess the appropriateness and necessity of medical services and expenses, thereby aiding in cost containment for the organization involved. This process encompasses various types of reviews, each playing a specific role in optimizing the balance between service volume and the quality of care provided. The key forms of utilization reviews include:
Pre-Admission Reviews for Scheduled Hospitalization (Precertification Review): This type of review occurs before scheduled hospitalizations, ensuring that pre-approval, or precertification, is obtained. It is designed to determine the necessity of planned medical treatments.
Admission Reviews for Unscheduled Hospitalization (Precertification Review): Similar to pre-admission reviews, this process focuses on unscheduled hospitalizations, requiring precertification to assess the necessity of the medical services.
Second Opinions for Elective Surgeries: In cases of elective surgeries, a second opinion may be sought as part of the utilization review process to ensure the appropriateness and necessity of the proposed procedure.
Concurrent Reviews: These reviews are conducted during the course of treatment to assess ongoing medical necessity and appropriateness, ensuring that the care provided aligns with established guidelines.
Individual Case Retrospective Reviews: After the provision of medical services, individual case retrospective reviews evaluate the appropriateness and necessity of the care rendered, retrospectively analyzing the course of treatment.
Aggregate Plan Retrospective Reviews: This form of review assesses the overall effectiveness and appropriateness of the healthcare plan, considering the cumulative impact of various individual cases.
These reviews involve collaboration between healthcare professionals, doctors, and insurance companies, and may also be conducted by independent agencies. Striking a delicate balance between reducing service volume and enhancing the quality of care is a critical consideration in the utilization review process.
One crucial aspect of utilization review is the precertification review, a pre-approval process mandated by insurance companies for specific treatments. Procedures requiring precertification often include non emergency hospitalization, outpatient surgery, skilled nursing and rehabilitation services, home care services, and home medical equipment. The review and approval process meticulously assess whether the requested service is medically necessary, serving as a crucial step in the comprehensive utilization review framework.
Many insurance plans follow pre-established clinical guidelines for specific conditions, employing a thorough process known as utilization review. This involves two primary types: pre-approval reviews and concurrent reviews.
In pre-approval reviews, the insurance committee evaluates submitted precertification requests against established guidelines. They collect comprehensive data, including symptoms, diagnostic results, and relevant medical information, comparing it to the plan's benchmarks for medical necessity. The committee may communicate with healthcare providers and other experts to make well-informed determinations.
Concurrent reviews come into play during active management of a medical condition, ensuring timely and cost-effective care. Physicians submit new treatments, along with detailed information on procedures, clinical status, and progress, for approval. The goal is to provide the correct care promptly, and the insurance company communicates its decision to the healthcare providers.
A crucial aspect of concurrent reviews is assessing the need for continuous hospitalization, aiming to minimize hospital stay duration. Feedback often includes specific discharge plans, which may be adjusted based on treatment complications or abnormal test results, emphasizing the importance of cost containment.
Retrospective reviews occur after treatment completion and serve two purposes. Individual case reviews may approve or deny coverage for already-received treatments, comparing specific elements to similar cases and potentially revising guidelines. Emergency cases, like acute care surgeries, may undergo this review before any payments are made.
Aggregate group reviews involve analyzing statistics on incident experiences, providing plan sponsors with average data compared to benchmarks. Plan sponsors, responsible for all medical costs in employer-sponsored plans, rely on intermediaries and empirical data to manage expenses effectively. Utilization management, often synonymous with utilization review, plays a vital role in this process, utilizing advancements in information technology to support cost-containment efforts through utilization improvement and adherence to evidence-based medical practices.
Value-Based Benefit Design
Recently, a noteworthy addition to healthcare benefits has emerged — the value-based benefits design (VBBD). This innovative approach, akin to previously discussed features, is strategically crafted to address the escalating costs in healthcare. What sets value-based design apart is its emphasis on delivering services that prioritize value over conventional offerings.
Under the VBBD program, employees are incentivized to opt for services offered by high-performing healthcare providers. These incentives span a spectrum, encompassing rewards, reduced premium costs, adjustments to deductibles and copays, and contributions to tax-advantaged funding plans such as Health Savings Accounts (HSAs).
Guided by a set of principles, value-based benefit design operates on the following tenets:
Measurement of healthcare value based on the medical benefits derived from prescribed treatments.
Preference for high-performance providers adhering to evidence-based treatment guidelines.
Emphasis on high-value services, spanning specific prescription drugs and preventive care measures.
Recognition of healthcare services differentiated by the quality of medical intervention provided.
Acknowledgment that the individual healthcare consumer contributes to value through healthy lifestyle choices, including increased physical activity and smoking cessation.
The outcomes of a VBBD program are gauged through the medical evidence of treatment effectiveness, the associated cost, and the resulting benefit of the treatment. Recognizing the variability in the value of services to each individual, VBBD advocates for cost sharing among enrollees based on the net value of the service to each employee. This underscores a departure from uniform costs for all employees or static pricing models.
In the realm of health insurance design, VBBD suggests a tiered cost approach for services, while prescription drugs align with efficacy considerations. Office visit copays, similarly rooted in efficacy, contribute to this tier-based system designed to guide employees toward choices that enhance the overall benefits package. This nuanced approach ensures that the value-based benefits design not only manages costs but also directs individuals towards superior healthcare choices.
Research has conclusively shown that financial incentives wield a considerable influence on health-related behavior, and the costs associated with services and prescribed drugs significantly affect their utilization. Thus, the strategic objective of VBBD initiatives is to enhance the probability of employee adherence to recommended treatment plans and the adoption of healthier behaviors. It is worth noting that individuals who prioritize their health generally incur lower overall healthcare costs. Furthermore, evidence suggests that patients managing specific chronic conditions while adhering to prescribed regimens also tend to experience reduced overall healthcare costs. The removal of barriers to valuable services and the incorporation of positive incentives within VBBD initiatives are pivotal in fostering a healthcare landscape where individuals are more likely to embrace recommended treatments and cultivate health-conscious behaviors.
Differentiating VBBD from CDHD and Value-Based Purchasing
A VBBD plan fundamentally diverges from a CDHP (Consumer-Driven Health Plan). In a CDHP, often referred to as a high-deductible plan, the enrollee bears the responsibility for service costs and the deductible, fostering heightened cost awareness and providing additional motivation for the enrollee to assess value judiciously. In contrast, a VBBD plan seamlessly integrates the concept of value into its incentive structure. Notably, a VBBD plan avoids the potential risks associated with CDHPs, such as the peril of deferring essential services to evade the full cost or accumulating balances in a tax-deferred account.
The National Business Coalitions' report, titled "Value-Based Benefit Design: A Purchaser’s Guide," provides a strategic roadmap for the implementation of such plans. This comprehensive guide outlines essential steps for effectively incorporating value-based benefit design into healthcare strategies.
Population Analysis:
The initial step involves meticulous data collection and analysis, encompassing information on medical claims and prescription drugs. The objective is to pinpoint areas susceptible to losses from health issues, which can be mitigated through treatment tracking and enhancements in healthy lifestyles. Medical professionals should scrutinize this data to make informed decisions. After analysis, a strategic decision is made on which employee segment should be the focus of the VBBD program. This precision allows incentives to be directed at specific providers and employees, ensuring that only those with particular conditions are motivated to seek specific services. To optimize this targeting effort, collaboration with a clinical decision support organization is essential, providing expertise in identifying the optimum target population.
VBBD Plan Development:
With the collected data as a foundation, the plan sponsor proceeds to develop the program's initiative, directly aligning with the insights gained in the previous step. For instance, if there's a substantial group of diabetic employees exhibiting noncompliance with healthy lifestyle guidelines or drug regimens, the VBBD program should be tailored to enhance positive outcomes related to diabetes. Notably, strict adherence to a drug regimen directly correlates with reduced healthcare costs.
Key elements in this strategic phase involve imposing financial constraints on high-value services and offering positive incentives for lifestyle changes. High-value services, proven to closely correlate with improved health, are prioritized. Features of a VBBD plan reducing copayment amounts for prescription drugs and equipment include:
a. Reducing copayments for specific drugs or equipment when used in disease management programs.
b. Lowering copayment amounts for office visits billed as wellness visits.
c. Adjusting deductibles for completing a personal health assessment (PHA).
d. Modifying deductibles for participating in disease-management or wellness programs.
e. Reducing copayment amounts for utilizing high-quality services.
Common positive incentives include:
a. Lowered premium contributions for completing a PHA.
b. Reduced premium contributions for smoking cessation.
c. Premium contribution reduction for participating in disease-management or wellness programs.
d. Contributions to an employee’s HSA for completing a PHA.
e. HSA contributions for participation in disease-management or wellness programs.
Vital to the success of a VBBD program is robust support and education. Plan sponsors collaborate with vendors to establish a support system for employees, offering disease management, case management, and health coaching as needed. Given the complexity, starting with a pilot program before widespread implementation is often advisable.
Developing a Communication Program:
Crafting an enduring and impactful communication program is paramount, given the novelty of the VBBD concept. Recognizing that employees may take time to fully comprehend the program's intricacies, a well-designed communication strategy should span up to a year. Participants often grapple with the notion that high-quality services can be more cost-effective, emphasizing the need for consistent messaging. Senior management endorsement is pivotal and should be consistently leveraged to reinforce the system's importance.
Vendor Management:
Effective management of vendors is a critical facet of successful VBBD implementation. Given the reliance on multiple vendors in a VBBD program, the sponsor must institute a robust vendor management framework. Clear articulation of program objectives and solutions is imperative for all vendors. Well-defined procedures should govern vendor communication and facilitate efficient problem identification and resolution. A structured vendor evaluation system, complete with established performance standards, adds a layer of accountability to ensure the seamless operation of the VBBD program.
Legal and Regulatory Framework
It is crucial to recognize that a VBBD program, like many other benefit programs, is subject to stringent legal compliance requirements, encompassing:
HIPAA Privacy Requirements: The handling of personal health information must adhere to the rigorous privacy standards mandated by the Health Insurance Portability and Accountability Act (HIPAA).
State/Federal Confidentiality Requirements: Any discussions pertaining to health conditions must align with the confidentiality stipulations laid out by state and federal regulations.
Communication of Confidentiality Protection: It is incumbent upon the program administrators to effectively communicate the measures taken to safeguard confidentiality to all employees, fostering trust and compliance.
Legality of Including Preventative Services for Chronic Diseases in HSAs: In cases where VBBD initiatives involve health savings accounts (HSAs), a thorough investigation into the legal implications of incorporating preventative services for chronic diseases is imperative. This ensures compliance with relevant laws and regulations governing such financial arrangements.
• Another critical consideration is the potential issue of discrimination inherent in the nature of the VBBD plan. While evidence indicates that plan participants typically do not perceive such a plan as discriminatory, it is imperative for the plan sponsor to disseminate all objectives and specific nuances of the plan extensively. Achieving a widespread understanding of the program among employees is essential to address any concerns and foster transparency in the implementation of the VBBD plan.
Concluding Thoughts on Healthcare Benefits
As we wrap up this chapter, let's reflect on the pressing issues influencing healthcare finance today. As explored both here and in Chapter 2, the paramount concern is healthcare cost containment. The unrelenting escalation of healthcare costs, albeit to a somewhat lesser extent currently, necessitates a comprehensive financial and economic analysis to benefit the entire healthcare industry.
Compounding the intricacies of this subject is the general lack of consumer knowledge about the healthcare product they are acquiring. Often, individuals are spending other people's money facilitated through third-party payments, adding to the overall complexity.
Expenditures in healthcare have seen substantial increases and are projected to persist on this trajectory, albeit at a somewhat decelerated pace. Amidst this landscape, health insurance financing remains the primary mechanism for funding healthcare benefit programs. The efficacy of insurance lies in risk pooling, and consumers' risk aversion underscores their approach to purchasing insurance. However, the specter of adverse selection poses a potential threat to the viability of insurance markets. Additionally, the concept of moral hazard introduces the risk of losses stemming from excessive consumption. Navigating these challenges demands a nuanced understanding of healthcare finance dynamics and a strategic approach to address the intricacies of this vital industry.
To encapsulate recent trends in health financing, the following key developments have emerged:
Shift from Indemnity Fee-for-Purpose Plans to Managed-Care Plans (PPOs and HMOs): There has been a notable transition from traditional indemnity fee-for-service plans to more structured managed-care plans such as Preferred Provider Organizations (PPOs) and Health Maintenance Organizations (HMOs).
Adoption of Insurance Benefits with Higher Deductibles and Copays, Along with Medical Savings Accounts: There is a growing trend towards implementing insurance benefits featuring elevated deductibles and copays. Additionally, the integration of medical savings accounts allows individuals to benefit from tax deductions for out-of-pocket payments.
Increased Consumer Demand for Improved Drugs: The liberalization of pharmaceutical advertising has empowered consumers, prompting a more discerning approach to drug choices. This shift reflects a heightened expectation for access to enhanced medications.
Growing Role of Medical Technology in Healthcare: Medical technology is playing, and is anticipated to play an even more significant role in general healthcare. The widespread and rapid integration of medical technology has contributed substantially to the overall increase in healthcare expenses.
The prevailing consensus among healthcare specialists is that costs can be effectively contained or reduced through a strategic combination of the following three elements:
Decreasing the Utilization of Healthcare Services
Adjusting Reimbursement for Services
Reducing Overall Expenses Across the Entire System
This recognition underscores the multifaceted approach required to address the complex landscape of health financing and pave the way for sustainable cost management in the healthcare sector.
Decreasing the Use of Healthcare Services
Several measures can be implemented to decrease the use of healthcare services, with many involving access limitations. Historically, insurance companies have restricted coverage for those likely to require care, such as individuals with preexisting conditions. The Affordable Care Act has intervened to curb such practices, bringing about significant changes.
Payers can also employ strategies to increase out-of-pocket costs, encouraging patients to proactively limit their healthcare use. These measures may include:
Limiting Type and Number of Reimbursed Visits: Restricting the variety and quantity of reimbursed visits, such as those for mental health care or physical therapy.
Increasing Deductibles and Copayments: Raising the financial responsibility of patients through higher deductibles and copayments.
Decreasing Allowable Accounts for Procedures: Setting limits on the financial coverage for specific procedures.
Establishing or Decreasing Maximum Lifetime Expenditures: Regulating the maximum lifetime expenditure, influencing long-term healthcare costs.
While these strategies have shown effectiveness in reducing healthcare use, evidence suggests that patients may not only avoid unnecessary care but also forego necessary care. Administrative hurdles, such as requiring approvals for tests, referrals, and procedures, contribute to a slight decrease in use without outright denial of care.
However, limiting access to healthcare presents its own challenges. Denying care to individuals often results in serious illnesses, which, when untreated, may lead to emergency room admissions. This poses a financial burden on the healthcare system, especially when uncompensated, potentially outweighing the cost of initial routine care. The Affordable Care Act addressed these issues by emphasizing comprehensive care provision.
Efforts to eliminate unnecessary care involve defining and recognizing practices that do not improve patient outcomes. This involves extensive studies of comparative effectiveness and cost-effectiveness to identify best practices. Comparative effectiveness studies extend beyond drug usage to encompass exercise, physical therapy, various providers, care settings, and reimbursement systems. Education and monitoring of providers, coupled with enhanced service coordination through universally readable electronic medical records, contribute to reducing practice variations and increasing cost-effectiveness.
Encouraging the use of inexpensive preventive services, such as screenings and diabetes or hypertension treatment, can diminish the need for more costly interventions later. Strategies to promote preventative care include:
Incentives for Primary Care Physicians: Encouraging primary care physicians to provide screening measures and prevent complications.
Pay-for-Performance Measures: Rewarding adherence to preventive care guidelines.
Elimination of Copayments: Removing financial barriers by eliminating copayments for preventive procedures.
By implementing these measures, the healthcare system can strike a balance between cost control and comprehensive care, ultimately promoting efficiency and improving patient outcomes.
Decreasing Reimbursement for Care Used
Enhancing the efficiency of healthcare delivery, even in the presence of comprehensive healthcare coverage, involves implementing strategic measures to curtail expenditures. Some notable strategies include:
Negotiating Lower Fees:
Both government and private payers can engage in negotiations with healthcare providers to establish lower fees. In the United States, for instance, the influence of reimbursement rates set by Medicare/Medicaid can prompt adjustments in fees across various plans, potentially leading to a reduction in overall reimbursement.
Promoting Primary Care Utilization:
Encouraging the increased utilization of primary care services over specialty care can be instrumental in cost containment. The adoption of a patient-centered medical home model, where primary care practitioners coordinate and integrate all facets of patient care, aims to minimize unnecessary specialty and duplicative care. This approach aligns with individual health goals, potentially mitigating inappropriate interventions.
Prospective Payment Systems:
Implementing prospective payment systems involves compensating healthcare providers with a fixed amount, irrespective of the services rendered. This fixed amount can be determined based on a predefined number of care services or a set annual reimbursement per patient. For instance, Medicare uses Diagnosis-Related Groups (DRGs) to establish fixed payments linked to specific diagnoses. Capitated systems, another variant, allocate a fixed annual sum to providers for patient care, irrespective of service volume. While these systems incentivize cost-effective care, they may inadvertently discourage comprehensive care for patients with complex conditions or serious illnesses, potentially impacting the overall quality of care.
To address the potential drawbacks of cost containment strategies, quality control systems and professional review organizations are often established. These entities play a crucial role in monitoring and maintaining the standard of care provided, ensuring that necessary medical interventions are not compromised despite the emphasis on cost-effectiveness. Achieving a balance between fiscal responsibility and maintaining the quality of healthcare services remains a paramount objective in the ongoing evolution of healthcare delivery models.
Addressing challenges in the U.S. healthcare system involves confronting issues such as denial of claims, competition dynamics, and strategies for reducing costs, particularly in the realm of prescription drugs. Consider the following nuanced exploration:
Denial of Claims:
Unlike many developed nations, the United States experiences a notable frequency of insurance claim denials, reaching an average of approximately 30% in California in 2009. While some denied claims are eventually paid through appeals, the appeals process exacts a toll in terms of time and effort for patients, healthcare providers, and payers alike.
Competition Dynamics:
The landscape of competition among healthcare providers and insurance companies can foster price competition, ostensibly benefiting consumers. However, the lack of transparency regarding provider charges and the constraints on patient choices often limit the impact of this competition. Consumer awareness of provider charges is frequently inadequate, diminishing the effectiveness of market-driven forces. Additionally, the subsidization of medical care costs for consumers through employer-paid health insurance, tax deductions, and savings accounts may reduce the incentive for individuals to seek competitive prices. Effective competition is often more pronounced in dealings between large corporations, such as insurance companies vying for contracts with corporations and government agencies, and providers competing for contracts with insurance companies.
Cost Reduction Strategies in Drug Expenses:
Controlling drug costs is pivotal in mitigating overall healthcare expenses. Various strategies can be employed, including:
Educating healthcare providers on the judicious use of cost-effective drugs.
Imposing restrictions on drug marketing campaigns.
Implementing formularies and leveraging pharmacy benefit managers.
Authorizing government negotiations for drug prices on behalf of patients covered by government insurance.
Allowing the importation of drugs from other countries to introduce competition and cost savings.
Impact on Medical Research:
Financial support derived from clinical practice and drug sales is often instrumental in sustaining medical research in academic medical centers. Consequently, a decrease in reimbursement rates may precipitate a decline in medical research activities. It is crucial to recognize that if alternative funding sources, such as governmental or private grants, are utilized to compensate for reduced income from reimbursement, these funds must be factored into healthcare costs. This consideration underscores the complex interplay between financial incentives and the vitality of medical research within the healthcare system.
Decreasing Overhead Expenses
The term "overhead expenses" in healthcare refers to payments that do not directly contribute to healthcare providers, encompassing administrative costs, malpractice insurance, and corporate profits (particularly in for-profit hospitals and insurance companies).
Strategic approaches to reduce overhead expenses include:
Decreasing Payer Overhead:
In contrast to governmental healthcare plans and private health plans in many developed countries (averaging 3% to 5% of total costs), private insurers in the United States often exhibit higher overhead costs, ranging from 20% to 30%. This discrepancy is partially attributed to the extensive staffing required for underwriting, claims evaluation, denial decisions, and appeals adjudication. Strategies to mitigate these costs involve:
Promoting standardized electronic health records to streamline administrative processes.
Advocating for increased utilization of government plans and potentially nonprofit plans to enhance efficiency.
Encouraging competition among payers to foster efficiency improvements, although this must be balanced against the potential for increased claim denials.
Decreasing Provider Overhead:
Reforms targeting payers can alleviate provider overhead by eliminating the need for billing and claims personnel managing multiple payers. For instance, countries like Germany and Japan, with multiple insurance companies vying for business, implement measures such as:
Simplifying billing processes to reduce administrative burdens on healthcare providers.
Streamlining appeals and claims justification procedures.
Implementing such changes not only streamlines administrative processes but also contributes to a more efficient and cost-effective healthcare system.
Ensuring fairness and uniformity in healthcare payment structures is essential for fostering an equitable and efficient system. Consider the following principles:
Uniform Payment Standards:
Payment amounts and rules should be standardized across all insurance companies. This ensures consistency and eliminates disparities, creating a level playing field for both providers and insurers.
Universal Payer Responsibility:
It is imperative that payers are obligated to cover the bills of all healthcare providers. This universal responsibility promotes financial stability within the healthcare system, preventing undue burdens on individual providers and facilitating a more predictable revenue stream.
Nationwide Uniformity in Service Costs:
Standardizing the cost of services nationwide is a fundamental measure for promoting equity and transparency. When the costs for services remain uniform across the country, it not only simplifies financial planning for both providers and payers but also contributes to a more accessible and consistent healthcare experience for patients.
While malpractice costs constitute a fraction of overall healthcare expenses, their impact on certain physicians' annual income can be substantial. Initiating reforms to reduce the frequency of lawsuits and settlements is not only beneficial for physicians but also holds broader advantages:
Premium Reductions:
Lowering the incidence of legal actions against healthcare providers has the potential to reduce malpractice insurance premiums. This, in turn, safeguards a significant portion of physicians' income, allowing them to allocate resources more efficiently.
Incentive for Efficient Practices:
Reform measures aimed at curbing unnecessary lawsuits may also discourage the practice of defensive medicine—where physicians order extra tests or procedures to minimize legal risk. By addressing this issue, reforms contribute to more judicious and cost-effective medical decision-making.
Implementing such reforms not only serves the financial well-being of healthcare professionals but also aligns with broader goals of fostering a more cost-effective, patient-centered, and equitable healthcare system.
Summary
Throughout the preceding chapters, the central challenge in the realm of healthcare benefits has consistently revolved around the imperative to rein in escalating healthcare costs—a dilemma that persists, albeit to a somewhat reduced extent. The exorbitant nature of these costs underscores the critical need for rigorous financial and economic analyses within the healthcare industry.
Compounding the intricacies of this issue is the reality that a significant majority of healthcare consumers are navigating a landscape where they purchase a product with limited understanding, all while relying on third-party payments. Medical expenditures have undergone a remarkable surge and are poised to continue their ascent, albeit at a more moderate pace. As a cornerstone, health insurance financing persists as the primary mechanism for funding healthcare benefit programs. The efficacy of insurance hinges on the principle of risk-pooling, rooted in consumers' risk aversion, but the specter of adverse selection threatens the stability of insurance markets. Moreover, the concept of moral hazard introduces the potential for losses arising from excessive consumption of healthcare services.
In this complex and dynamic landscape, the necessity for astute financial and economic analyses becomes increasingly apparent. Addressing the challenges of cost containment, consumer understanding, and the intricacies of insurance dynamics demands a multifaceted approach that appreciates the interconnected nature of these factors. As we navigate the evolving terrain of healthcare benefits, the role of comprehensive analysis remains paramount in crafting effective and sustainable solutions.
Key Concepts in This Chapter
• Insurance-based financing
• Self-insured financing
• Employee Retirement Income Security Act (ERISA) and a self-funded plan
• Value-based benefit design (VBBD)
• Consumer-driven health plan (CDHP)
• Cost containment
Unit 2 Discussion
What are your thoughts on universal health care? Support your position.
I think universal health care can work but our current system and overall health really needs to be changed. Currently there's a sick culture that is the way doctors treat patients. And it also doesn't help that the FDA's regulation of chemicals that goes into food is more about just making sure people don't die right away from what's being put in food. An example is cellulose that you see in many different types of food is actually wood pulp. Saw dust contains about 40% cellulose and companies are using that as an ingredient in food but because there's no short term health effects its a safe product. Another example Titanium dioxide which is banned in Europe because it has the potential to damage the immune system and damage DNA cells but its found in candies, pastries, chewing gum, coffee creamers, chocolates, and cake decorations in the US and the FDA says its safe because of the small amount that you can potentially consume that it shouldn't effect people. But when you add the fact you often consume many products with that who can regulate exactly how much total your body accumulates it sure makes you think. If our society wasn't praying on the fact that we are likely going to have autoimmune diseases, and develop diabetes and other sickness from various chemicals in our foods to save money make products cheaper so companies can profit and doctors worked on preventative care and worked on trying to make people healthy rather then sick universal care done correctly would be beneficial. Like some of the best countries with health care like Denmark for example. But the way things are set up a universal healthcare could never be applied to our country and be a successful plan without a lot of changes having to be made.
Unit 2 Assignment - Health Care Plans
Referring to Unit 2 Readings and Resources, write a 4-5 page paper proposing a health care plan and include how you would finance the plan.
Your paper should include:
Cover page
4-5 pages of content
Reference page
When it
comes to healthcare each plan can be very different and also healthcare on a
whole falls short of many of the other countries since while health care can be
really good here it can also be very expensive and not cost effective for
everyone. And while Obama care attempted to give everyone cost effective health
care overall it just hurt healthcare in general. If I was to create a health
care plan, I would also look to fix the current healthcare system to support an
overall better plan that would be beneficial for all those that are seeking
health care.
One of the
first things I would do is first make cost a transparent number of patients.
Often when we get bills of medical procedures that we have had done we don’t
get any details of what the procedure charged for each individual cost we just
get an end price of the total. Also if you’ve ever had no insurance when
seeking medical aid like I have in the past. I’ve been charged the same amount
before with and without insurance meaning that often the doctor can get away on
some plans to double dip charging the patient the same amount saying this
wasn’t covered by the health insurance when the health insurance was billed the
exact same amount that was the overage amount. But because there’s no
transparency for billing or prices you also have no way of tracking or
disputing anything. Also changing transparency would also offer the option to
shop for a better overall care experience rather than having to shop in
specific networks and more competitive and better overall experience because
the better doctor with better care would be in higher demand making all doctors
strive for the same excellence.
Another
important change is stop incentivizing sick care. Doctors should care about
patients getting well and focus on a wider range of factors towards making
individuals healthy. Europe has many banned food additives that they won’t
accept food from the US unless it meets the strict requirements. Europe also
has a less sugar initiative requiring products to contain 25% less sugar in
soft drinks and soda to help reduce the potential health effects. If we cared
more about what chemicals and additives and the amount of sugar in products
here we could help reduce the number of sick individuals here there by also
preventing a larger amount of people needing extra care or continuation of care
such as diabetes. Doctors should be looking to see you less often and only when
care is required not for health conditions created by bad industry food
practices. And the FDA should be making sure food products contain real food
not wood pulp in food called “cellulose” that’s generally recognized as safe
and can be found in so many different foods but you won’t die tomorrow so it’s
considered a safe food product to use.
Another
area that could use to be improved is drug usage and allow more companies to
compete with safe generic drugs to help allow proper competition to markets so
drug companies hold less of a hold on consumers. There should never be
monopolies when it comes to healthcare pills and formulas even during
parenting there should be expiration of patents allowing more generic companies
to compete and also balance prices on drugs.
Of course
there’s many other ways to improve the current health care those changes would make
a pretty big difference on the overall healthcare system. In a situation like
that then a united healthcare system could be used in which a program better
than Obama care could be used. Rather than having many different companies for
health care one united healthcare plan could apply and could be used at
different levels depending on the type of care an individual requires. An
example of this would be an individual that is general healthy and doesn’t
often require care beyond preventative care and general health care such as
vaccinations, checkups general doctors’ visits but often doesn’t require
continual medication for a condition can have access to the benefits they need
and would have a balanced plan to fit those needs but also can cover them in the
event of any emergencies if something does happen. It can also include services
like health and wellbeing chiropractor's visits, gym membership and other
services which would help that individual maintain their overall health. A
healthy person would also be required to get a referral to see a specialist as
a result. As for a sick individual who often has continual medication
requirements but don’t often require more advanced procedures like surgeries
and such a plan for individuals with drug needs could be used to help maintain
those specific costs without adding the plan needs of someone with advanced
care. And lastly people who have a chronic condition or often require a lot of
medical and surgical care would fit in to the last category requiring the most amount
of care. And would not need referrals for specialists and such. Of course if
individual health situation improves from any of the plans they are in they
could switch to a different plan and the costs would then change based on those
needs especially if we are giving care that attempts to make sick people
healthy rather than prolonged care of sick people without a plan to make them
healthy to milk the healthcare system.
Cost is an
important factor when considering such a plan and also how to get the money for
such a plan. Obama care falls short in that the health care companies charge
more to the people who have money to pay for medical which is why Bluecross Blueshield
for example started to raise the cost to other members to cover the individuals
that where using Obama care and not having to pay out of pocket costs. Finding
a proper balance to help cover the costs of running a healthcare system is
important to the overall success.
As such
there should be overall health taxing service on all medical related but not at
the cost of the patients more like a network fee for doctors and providers they
are making money through the people who visit them and a percentage of that
should go back into the system covering the people. That includes all services
related to health and wellbeing. But requiring all individuals to have health
care or wellness care is important as well to help maintain that. So as a job
requirement all companies would need to require individuals to have health
insurance to help support the system as well. A portion of payment required by
the companies like normal would be required and instead of having to pick
outside companies it would be a united healthcare the government provides.
Taxation systems when it comes to healthcare work a perfect example of this is
that of Denmark which has a really great universal healthcare system that uses
regional and municipal taxation model and distributes that money to local
government. Though money gained through a system should not be able to be looted
for other outside purposes and should only be used on health care. That will
prevent the healthcare system from falling into a running out of money
situation similar to social security. If the health care system can’t be
touched for outside purposes it will be successful.
For it to
be completely successful it needs proper regulation and control and parties
that don’t meet strict requirements should be held responsible to ensure that
the patients always get a high level of care that is required to be maintained.
All of these changes as well as working towards making people stay healthy
would create a plan and a healthcare environment which would improve overall
healthcare for the US and help it compete with countries that are considered
the best in the world.


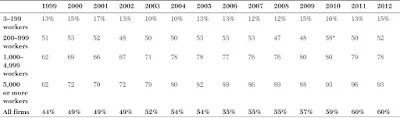
Comments
Post a Comment